Endovascular transvenous femoropopliteal bypass - can we forget about open arterial bypass?
The aim of Roberts Rumba's doctoral thesis was to determine the clinical, anatomical and venous physiological parameters and safety as well as efficacy of endovascular transvenous femoropopliteal (ETFP) bypass1 compared with open bypass in the treatment of long-segment superficial femoral artery occlusion.
Peripheral artery disease is prevalent throughout the world. It affects 13% of the world's population over the age of 50 and significantly increases the risk of mortality. Technological advances have made it possible to treat even complex, long occlusions (blockages) of the superficial femoral artery (SFA) endovascularly, but it is still difficult to decide which method is best for which patient. The advantage of endovascular revascularisation is its minimally invasive nature, which ensures a lower risk of complications and mortality, while open surgery is associated with a lower risk of major adverse limb events and better long-term survival. The new ETFP bypass combines the advantages of both approaches, allowing SFA revascularisation in cases where open bypass is not possible.
‘To date, this is the first and only study to evaluate ETFP bypass in Latvia. No other centre in the world performing this procedure has compared it with open femoropopliteal bypass in a vascular surgery unit. Furthermore, there are no publications on the physiology of the venous system in relation to the new bypass device. Other researchers have also published data on the clinical evaluation of the venous system, but our data obtained using plethysmography is unique. The novelty and practical value of the results obtained in my doctoral thesis is the data on vascular physiology and the direct comparison with open bypass control groups,’ says Roberts Rumba, author of the thesis.
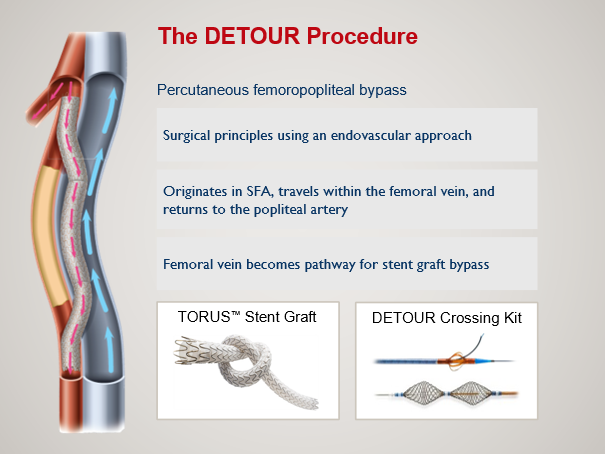 Image of an ETFP bypass
Image of an ETFP bypass
It is well known that not all clinical signs and symptoms indicative of venous disease are reflected by physiological changes in the venous system and vice versa. There are significant differences between the clinical assessment of the venous system and the results of objective measurements (plethysmography) performed in the doctoral thesis, which provide a more detailed understanding of the impact of ETFP bypass on the venous system of the lower extremities.
Firstly, the study evaluated the patients and procedures. This included the demographic and clinical parameters of patients who underwent ETFP bypass, an assessment of venous anatomy and physiological parameters at follow-up visits, and an investigation of the safety profile of ETFP and complications during surgery and in the post-operative period.
Secondly, an evaluation of efficacy and patency was performed: the efficacy of ETFP bypass in improving Rutherford classification2 and ankle-brachial index after surgery and the results of primary, primary assisted and secondary patency of ETFP grafts were evaluated.
Thirdly, a comparison with other methods was performed: the patency indicators of ETFP and open femoropopliteal bypass in patients with autovenous and synthetic prosthetic graft were compared.
Findings of the study
- ETFP bypass is a safe method with comparable efficacy to open bypass in the treatment of long-segment SFA occlusion.
- ETFP bypass does not cause long-term changes in venous symptoms and signs.
- Venous physiological parameters assessed by plethysmography remain unchanged after ETFP bypass.
- Primary, primary assisted and secondary patency rates for ETFP bypass are lower than for bypass but higher than for open bypass with a synthetic prosthesis.
Clinical recommendations and next steps
For patients who do not have a suitable vein for bypass and who have severe comorbidities, tissue damage and an increased risk of infection, ETFP bypass may be the best option. A good quality saphenous vein is the graft material of choice with the best long-term results in the treatment of long and complex SFA occlusions and should always be used in open surgery. Bypass with a synthetic graft should only be used in patients who have no other options for open or endovascular revascularisation. Heparin-containing prostheses are a reasonable choice when a large saphenous vein is not available. Duplex venography should be performed prior to any ETFP bypass procedure to assess the availability of a large saphenous vein or alternative autovenous material. Anti-platelet therapy is recommended after ETFP, and if clopidogrel resistance cannot be assessed, low-dose anticoagulation should be included during the first year after surgery.
‘This study is of both practical and scientific importance, as it will help to guide decision-making and tailor treatment to each patient and clinical situation. When the bypass device becomes available in everyday practice, we will already have experience and a large amount of data that we have collected ourselves, which will help in decision-making. We will be able to tailor the treatment to each patient and clinical situation, rather than relying on vascular surgery units in other countries or information provided by the device manufacturer,’ concludes Roberts Rumba.
1 New vascular bypass surgery using deep veins to bypass blocked arteries in the legs
2 The Rutherford Classification is a system used to assess the severity and stage of peripheral artery disease. This classification helps doctors determine how severe a patient's symptoms are and how serious the problem of blood flow to the legs is. The Rutherford Classification has several categories, ranging from asymptomatic disease to severe tissue damage and gangrene.
Related news
 Sports psychology study on young athletes: how burnout, anxiety, and wellbeing shape distinct athlete profiles Research, Psychology
Sports psychology study on young athletes: how burnout, anxiety, and wellbeing shape distinct athlete profiles Research, Psychology


