In Latvia, nasal polyps most often develop due to bacterial influence
Rūdolfs Jānis Vīksne is an otolaryngologist who has always been passionate not only about practical medicine but also about research. During his residency, he was surrounded by many young doctors who were deeply engaged in research, and gradually he, too, developed the desire to look deeper – not only to treat patients, but also to understand the causes and mechanisms of illnesses. Soon he arrived at the idea of studying nasal polyps, and this choice turned out to be both challenging and highly meaningful.

Rūdolfs Jānis Vīksne after defending his doctoral thesis
With the support of Associate Professor Gunta Segliņa and Professor Māra Pilmane, Rūdolfs gradually developed a research design, began collecting tissue samples at Pauls Stradiņš Clinical University Hospital, and learned various laboratory methods. Five years of work culminated in the successful defense of his doctoral thesis on the morphopathogenesis endotypes of nasal polyps – the first study of its kind in Latvia and the Baltics. It offers both scientific and practical value, helping to better understand the nature of the disease and potentially paving the way for more precise and effective treatment in the future.
Understanding chronic nasal inflammation
Chronic rhinosinusitis is a long-lasting inflammation of the nose and paranasal sinuses. People who suffer from it often experience nasal congestion, discharge, facial pressure, and impaired sense of smell. This significantly affects daily well-being and quality of life.
Rhinosinusitis can be divided into two forms: with nasal polyps and without them. Polyps are soft, benign tissue formations that develop in the nasal cavity and sinuses and make breathing difficult. Although there are many theories about their origin, there is still no definitive answer as to why these formations appear.
In recent years, scientists have increasingly focused on what exactly happens within tissues during inflammation, rather than only examining how the disease appears “from the outside.” These internal inflammatory characteristics are called endotypes. As a result, this topic has become one of the most important directions in modern research on nasal and ENT diseases.
Nasal polyp endotypes can differ greatly in various parts of the world. This means that people in, for example, Western Europe and Asia may develop polyps due to different inflammatory processes. Therefore, it was important to understand which types of inflammation are present specifically in Latvia.
Five nasal polyp endotypes identified
In the doctoral thesis, nasal polyp tissues from patients were compared with samples of healthy nasal mucosa. The study involved 48 patients with polyps – 29 with primary polyps and 19 with recurrent polyps (previously diagnosed and surgically treated). As control material, 17 samples from individuals with healthy nasal mucosa were used.
The tissue samples were processed at the RSU Morphology Laboratory using methods that allow detection of various inflammatory substances – cytokines, antimicrobial peptides, and cell proliferation markers. The results were first assessed under a microscope, then compiled and analysed statistically. This analysis made it possible not only to compare healthy tissues with polyp tissues, but also to determine which inflammatory mechanisms – endotypes – are characteristic of Latvian patients.
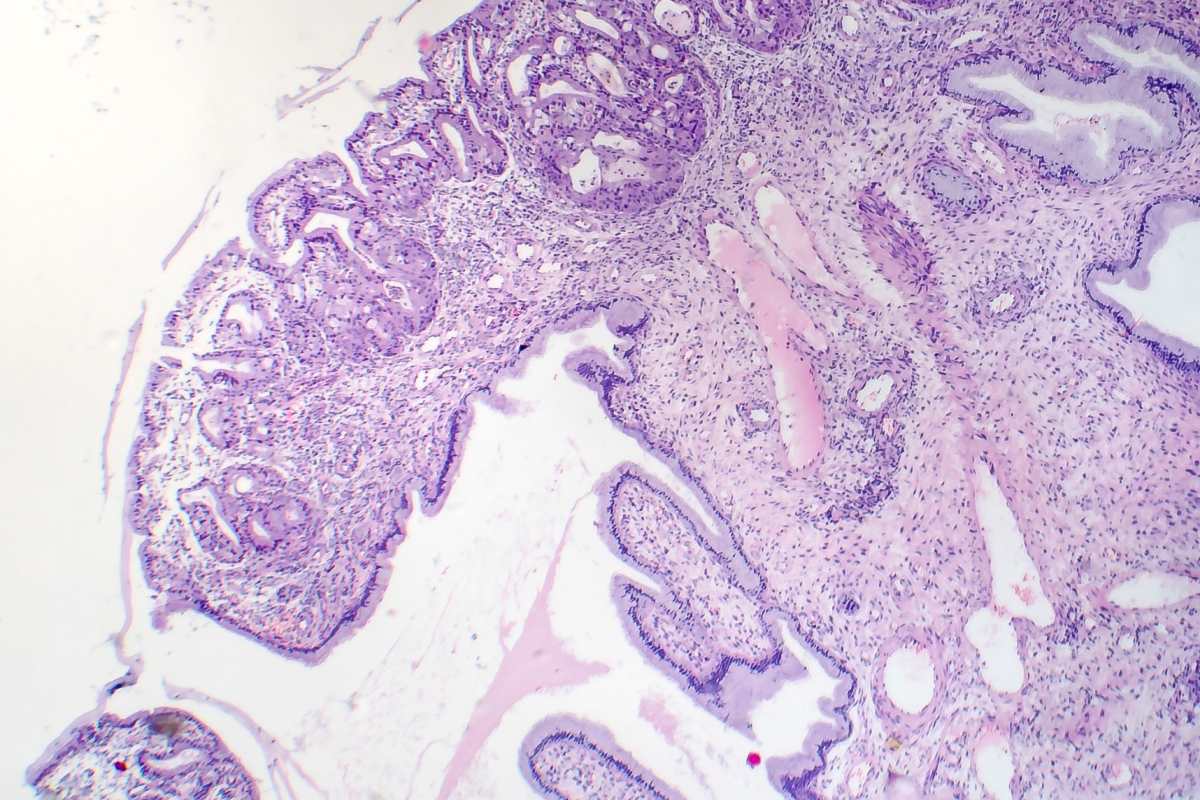
Microimage of normal nasal mucosa
The study showed that significant changes occur in nasal polyp tissues. One of the most important findings is that the epithelial protective barrier is impaired. In healthy nasal mucosa, most protective factors are found directly in the epithelium – the outer tissue layer. In polyps, these factors almost disappear from the epithelium and move into deeper tissues, indicating a weakened barrier and uncontrolled inflammation.
It was also found that the inflammatory cytokine IL-6 plays an especially important role, as it was elevated in both primary and recurrent polyps. The recurrent polyp group also showed increased IL-1α levels and more frequent asthma occurrence, suggesting a more severe disease course.
By analysing the extensive dataset, the study identified five distinct nasal polyp inflammatory endotypes. The most common endotype in Latvia is associated with neutrophilic inflammation and high levels of antimicrobial peptides such as LL37 and HBD-3. This indicates that bacteria may play a significant role in maintaining inflammation for a portion of patients.
A path toward personalised treatment of nasal polyps
Currently, treatments for nasal polyps worldwide are limited. Corticosteroid therapy –using nasal sprays or short-term oral courses – or long-term antibiotics are typically used. Only when these options no longer help is surgery considered. Rūdolfs Jānis Vīksne also emphasises that surgery is a last resort due to its risks – many operations can lead to adhesions, reduced mucosal function, and more complicated recovery.
In more severe cases, biological medications are used to suppress specific inflammatory processes. However, no method is universal – polyps often recur because each patient’s inflammatory mechanism may differ.
This is where the study’s results gain practical value. Knowing the patient’s specific endotype will make it possible to tailor treatment much more precisely. If the inflammation is primarily maintained by bacteria, longer courses of antibiotics may be appropriate. For patients with predominantly type 2 inflammation, biological medications may be more effective. This is a crucial step toward personalised medicine – an approach in which treatment is adapted to the patient’s specific inflammatory profile rather than applying the same therapy to everyone.




