RSU Medical Students Get Involved in Fight Against COVID-19
Arnolds Jānis Krauklis is a 3rd-year Medicine student at Rīga Stradiņš University (RSU). He is one of many students who have joined the experienced doctors at Pauls Stradiņš Clinical University Hospital and has been working as a hospital attendant at the Emergency Medicine Centre since September.
Although Arnolds is optimistic and believes that the current struggles are temporary, he is also concerned about the growing number of people infected with COVID-19, burnout among doctors, and the availability of services for patients with other illnesses.
‘I applied to work at Pauls Stradiņš University Clinical Hospital in order to get some practical experience, and it was here that I realised that I had chosen the right profession. Helping people is very satisfying,’ he says.
What is your day like?
As several colleagues have fallen ill, we are currently on 24-hour shifts. My shift begins at 8:00 in the morning and ends at 8:00 the next morning.
In order to arrive at the hospital on time, I have to wake up shortly after 6:00. I work as a hospital assistant in the medical admissions unit. There are five posts here with one hospital attendant at each. It is my duty to take care of patients. Some patients need help getting dressed, others to eat. I do not complain. At night, I can sleep for three hours.
No two patients are alike, and for some it’s the first time they’re admitted. I see the importance of a human conversation in a crisis situation as it helps people overcome their fears and to feel more at ease. It has been scientifically proven that patients’ psycho-emotional state affects the outcome of their recovery. Hotels want their guests to enjoy their stay, and I always keep this in mind when I interact with my patients.
What has been the hardest part of working in a hospital so far?
Facing death. This happens often. I understand that this is inevitable, but it is difficult to experience anyway. I have looked into the subject, and we had an elective course called Death and Dying at RSU, which helped me take a more philosophical look at this process. Death comes sooner or later, and there’s nothing we can do to change this. People spend their lives in fear of something that is inevitable.
I once got to talk to an older gentleman who had a serious disease. There was no sorrow, fear, or remorse in his eyes. He told me about his struggle with the disease and how he had once overcome it. He told me that people should enjoy the time they are given. After the first recovery, he travelled the world, enjoyed life and played sports, but when the disease returned, he was happy with what he had experienced. After a conversation like this, I can return home feeling peaceful. He was ready for whatever was to happen next.
What is it like to be working in a hospital during the COVID-19 pandemic?
I have to say that it depends - some days more patients are brought in, some days fewer. I witnessed a situation when the department received a call about a patient who was being taken to hospital in a very serious condition. The patient needed resuscitation, but the resuscitation room was full, however. After witnessing something like this I am amazed that there are still people who insist that COVID-19 does not exist.
The staff get sick, too. One day, I was suddenly afraid that I might get sick, and not because I was afraid of the disease, but because I would have had to give my shifts to my colleagues, and we were already understaffed. Two colleagues went home at night because they felt sick. The workload immediately increased – both emotionally and physically. This made me think about how else I might protect myself from the virus. In the last few days I have felt the consequences from the heavy workload – my back aches from being on my feet for such long hours and from lifting patients. There are many shifts and the pressure is high. I fear that if my colleagues can’t cope with the workload they might start resigning and just leave. People are burned out both emotionally and physically.
Have you ever heard any comments from a COVID-19 denier after they have received a positive test result at a hospital?
COVID-19 deniers don't talk that much once they contract the virus. We don’t hear any of this in the hospital.
What are the greatest challenges in the fight against COVID-19?
Right now, the most painful thing is the public's disbelief in COVID-19 and the fact that people do not follow the restrictions.
This is not just about COVID-19, but also about patients with other conditions. The public needs to understand that as the number of people who are hospitalised with COVID-19 increases, others will have less access to medical care. I once asked a man if he had any idea where he got the virus. He had been staying at home and only occasionally gone to the store, but his son and his wife had come to visit and they tested positive.
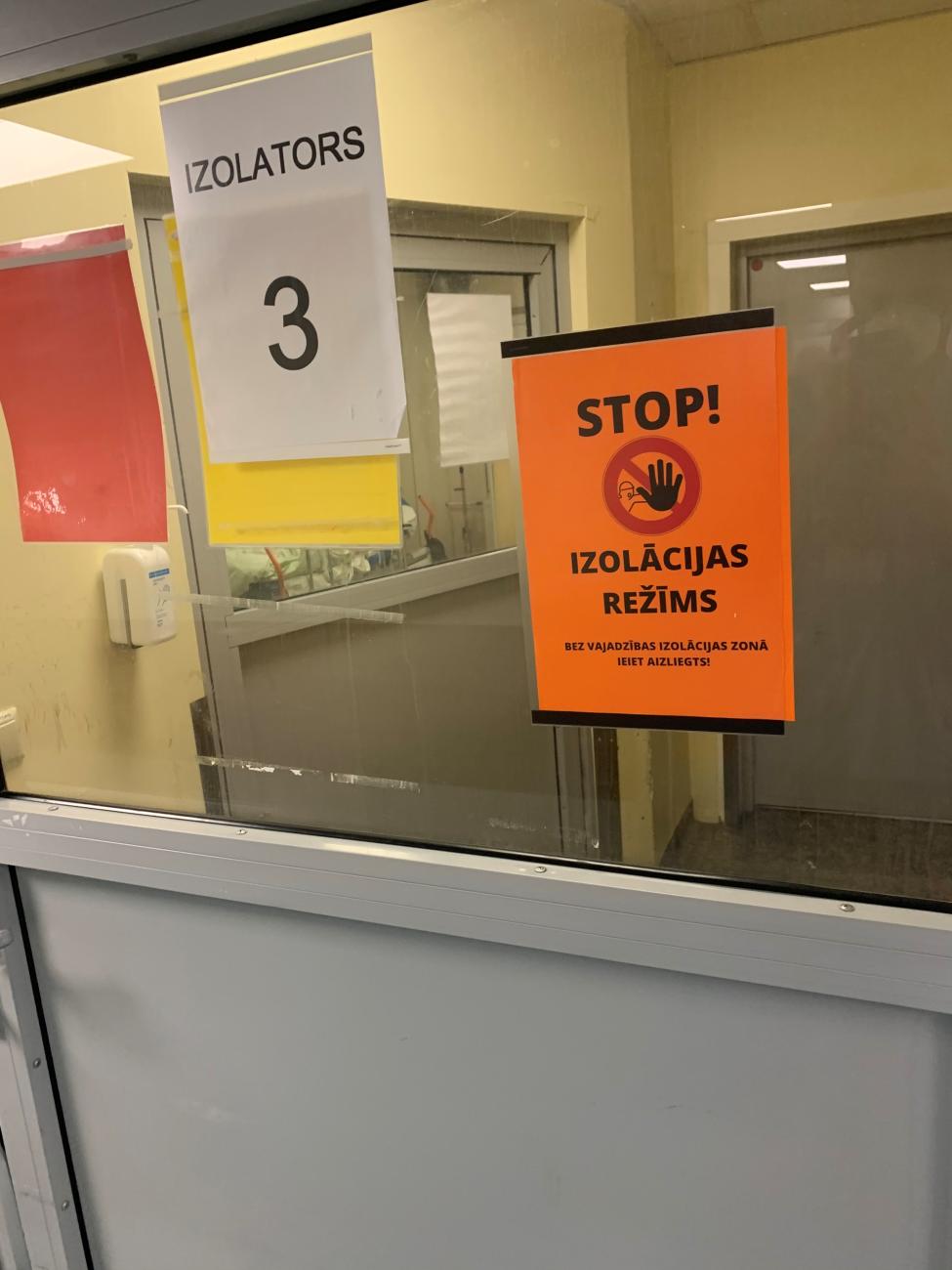
Working in personal protective equipment is challenging – it feels like you have a heater inside. I only need to put it on at certain times where I work, but my colleagues who work in the COVID-19 wards wear them all day. It's hard for me to imagine what that must be like.
As a prospective doctor, do you have anything to say to your peers?
Don't give up! There will always be difficulties like COVID-19, one way or another. Our own actions and attitude are the key. In five years, we will be able to look back at this as a valuable lesson, but for now – observe the restrictions, do not meet with others, and do not visit your relatives or friends.
Please do your part so the doctors can do theirs! Stay at home!