Prevalence of Actinic Keratosis and Its Associated Risk Factors in Elderly Latvian People
Abstract
Actinic keratosis (AK) is a frequent skin lesion that affects millions of patients worldwide and is becoming the most common in situ carcinoma in humans. Independent risk factors for AKs include older age, male gender, cumulative sun exposure, artificial UV radiation and Fitzpatrick skin types I and II. According to the World Health Organisation (WHO), the estimated prevalence by latitudinal band in Latvia could be 5–8 % in men and 2.5–4 % in women older than 60 years. The aim of this study was to determine the prevalence of actinic keratosis and its associated risk factors among elderly Latvian people. To achieve the aim, questionnaires from skin cancer screening campaign were gathered and analysed. Only patients above the age of 60 that had received full body examination were included in this study.
Actinic keratoses were diagnosed in 51.8 % of study participants, with higher, but not statistically significant prevalence in men (62.5 % vs. 47.4 %, p = 0.057). The prevalence of UV related risk factors was high – 70.2 % of participants had skin phototype I or II, almost half of the participants (46.6 %) had had severe sunburns before the age of 18, 21.6 % had had an outdoor job, 77.4 % had spent more than two weeks per year relaxing in the sun, while only 6.9% of the participants always used sunscreens while sunbathing. The study also showed that actinic keratoses were more prevalent among participants that had had severe sunburns before the age of 18 (64.0 % vs. 41.2 %; p < 0.01) and among participants that had spent more than two weeks per year relaxing in the sun (56.5 % vs. 37.2 %; p = 0.026).
This study suggests that prevalence of actinic keratosis might be higher in Latvian population than previously expected and highlights the necessity to protect skin from UV radiation in order to diminish the prevalence of AK.
Introduction
Actinic keratoses (AK) are keratotic lesions occurring on chronically light-exposed adult skin (Berker, 2007). Historically AK have been defined as “precancerous” or “premalignant”, but more recent histopathologic and molecular studies support their current classification as the earliest stage of squamous cell carcinoma in situ (Röwert-Huber, 2007; Zalaudek, 2014; Ferrándiz, 2013). European guidelines of this disease concluded that AK are increasing in prevalence; it affects millions of patients worldwide and is becoming the most common in situ carcinoma in humans (Ferrándiz, 2013). Despite the fact that they are frequent, they are not well recognised by public (MacKie, 2004). Independent risk factors for AKs include older age, male gender, cumulative sun exposure, artificial UV radiation and Fitzpatrick skin types I and II (Rosen, 2013, Ferrándiz, 2013). Recent study also indicates baldness in men as the strongest risk factor for the development of AKs (Flohil, 2013). There are not many prevalence studies in Europe especially in elderly population. The prevalence of AK in Latvian population has not been previously studied. According to the World Health Organisation (WHO), the estimated prevalence by latitudinal band in Latvia could be 5–8 % in men and 2.5–4 % in women older than 60 years (Lucas, 2006).
Aim
The aim of this study was to determine the prevalence of actinic keratosis and its associated risk factors among elderly Latvian people.
Material and Methods
To achieve the aim, questionnaires from skin cancer screening campaign, which took place from September 9 to October 6, 2013, were gathered and analysed. During this campaign doctors from nine cities representing different Latvian regions screened voluntary patients for all types of skin lesions and asked questions about previous sun exposure and sun protection habits. Only patients above the age of 60 that had received full body examination were included in this study. All questions were asked and skin examinations performed in health care centres in a single visit, and dermatoscopy was used to confirm the diagnosis. Questionnaires were filled with the following data: patient’s gender, age, skin Fitzpatrick phototype and lifetime sun exposure. The later included such questions as whether the person had ever had an outdoor job; whether they had ever spent more than a year in a country with a higher UV index than Latvia; whether they had ever had severe sunburns before the age of 18 (sunburns with painful blisters or erythema lasting for more than 2 days); whether they used sunscreens while being in the sun for more than an hour and weather they used them while sunbathing; whether they had ever used a sunbed and what the average amount of weeks they spent in sun every year had been. Whenever possible it was asked to estimate the amount. Oral consent was obtained from all patients.
Statistical associations between the presence of actinic keratoses and risk factors were tested with Pearson’s chi-square test, Fisher’s Exact Test or Mann–Whitney U test. Results are described as numbers and percentages for categorical variables, means ± standard deviations for continuous variables. The level of significance was set at 0.05. All analyses were performed using IBM SPSS 20.0.
The study was approved by the Ethics Committee of Rīga Stradiņš University (permit issued on 28.11.2013.).
Results
A total number of 191 patients were included in this study. Female accounted for 70.7 %, while male accounted for 29.3 %. Their age ranged from 60 to 94 years (mean ± standard deviation: 74.0 ± 7.7 years).
Actinic keratoses were diagnosed in 51.8 % of study participants, with higher, but not statistically significant prevalence in men (62.5 % vs. 47.4 %; p = 0.057, Pearson’s chi-squared test). Prevalence of AKs rose with age in both genders (Figure 1) ranging from 29.5% in 60 to 69 year-old group, to 57.9 % in 70–79 year-olds, to 68.5 % in study participants more than 80 years old.
This study showed a high prevalence of most risk factors – 70.2 % of all participants had skin phototype I or II, 21.6 % had had an outdoor job, 46.6 % had had severe sunburns before the age of 18, 10.6 % had lived in a country with a higher average UV index than Latvia for more than a year, 77.4 % had spent more than two weeks per year relaxing in the sun, 12.6 % had a history of skin cancer and only 6.9 % always used sunscreens while sunbathing and 2.6 % while being outdoors for more than an hour. The least prevalent risk factor was use of sunbeds – only 5.8 % of participants acknowledged ever using them.
In the group of participants that had had severe sunburns before being 18 years old, 64.0 % had actinic keratoses, in comparison with 41.2 % of those that had not had such sunburns. This association was statistically significant (p < 0.01, Pearson’s chi-squared test). Severe sunburns before the age of 18 increased the risk of AK 2.55 fold (OR = 2.545, 95 % CI: 1.417–4.570). In the group of participants that had had one to two severe sunburns before the age of 18, 42.9 % had actinic keratosis in comparison with 78.2 % of participants that had had three or more severe sunburns before the age of 18 (p < 0.01, Pearson’s chi-squared test). The risk of actinic keratoses was 4.78 times higher in participants that had had 3 or more sunburns before the age of 18 in comparison with those that had fewer sunburns (OR = 4.778, 95 % CI: 1.785–12.790).
Actinic keratoses were detected in 56.5 % of participants that had spent more than two weeks per year relaxing in the sun and in 37.2 % of participants that had spent less than that. This difference was statistically significant (p = 0.026, Pearson’s chi-squared test). More than two weeks per year relaxing in the sun resulted in a twofold increased risk of AK (OR = 2.188, 95 % CI: 1.088–4.403).
Skin phototype, outdoor job, more than a year spent in a country with a higher UV index than Latvia, use of sunscreens, use of sunbeds and skin cancer history was not significantly associated with increased risk for actinic keratoses. Associations between patient and UV risk factors and presence of AK are presented in Table 1.
Figure 1. Prevalence of actinic keratosis stratified by age group and gender
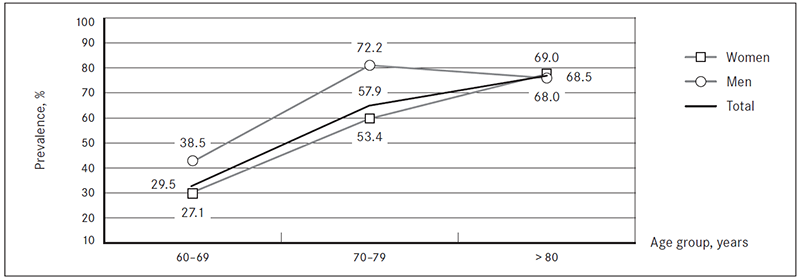
Table 1. Prevalence of AK according to patient and UV risk factors
| Risk factor | From total study population, N (%) | With AK, n (%) | p-value | OR | 95 % CI |
|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 |
| Gender | |||||
| Men | 56 (29.3) | 35 (62.5) | 0.057 | 0.541 | 0.286–1.023 |
| Women | 135 (70.7) | 64 (47.4) | |||
| Skin phototype (in comparison to “phototype I”) | |||||
| I | 21 (11.0) | 12 (57.1) | — | — | — |
| II | 113 (59.2) | 58 (51.3) | 0.624 | 0.791 | 0.309–2.024 |
| III | 57 (29.8) | 29 (50.9) | 0.623 | 0.777 | 0.283–2.129 |
| Outdoor job (in comparison to “no outdoor job”) | |||||
| Total | 41 (21.6) | 17 (41.5) | 0.123 | 0.579 | 0.287–1.166 |
| < 1 year | 4 (2.1) | 2 (50.0) | 1.000 | 0.817 | 0.112–5.956 |
| 2–5 years | 11 (5.8) | 4 (36.4) | 0.348 | 0.467 | 0.131–1.663 |
| 6–10 years | 6 (3.2) | 4 (66.7) | 0.693 | 1.634 | 0.290–9.197 |
| > 10 years | 20 (10.5) | 7 (35.0) | 0.092 | 0.440 | 0.166–1.165 |
| Severe sunburns before the age of 18 | |||||
| 89 (46.6) | 57 (64.0) | 0.002* | 2.545 | 1.417–4.570 | |
| Severe sunburns before the age of 18 (“1–2 times” in comparison to “3 or more times”) | |||||
| 1–2 times | 28 (33.7) | 12 (42.9) | 0.001* | 4.778 | 1.785–12.790 |
| 3 or more | 55 (66.3) | 43 (78.2) | |||
| Sunscreen use while being outdoors > 1 hour (in comparison to “never”) | |||||
| Always | 5 (2.6) | 3 (60.0) | 1.000 | 1.319 | 0.214–8.115 |
| Occasionally | 29 (15.2) | 13 (44.8) | 0.407 | 0.715 | 0.322–1.585 |
| Never | 156 (81.7) | 83 (53.2) | — | — | — |
| Sunscreen use while sunbathing (in comparison to “never”) | |||||
| Always | 13 (6.9) | 5 (38.5) | 0.387 | 0.543 | 0.169–1.751 |
| Occasionally | 47 (24.9) | 24 (51.1) | 0.776 | 0.907 | 0.465–1.770 |
| Never | 129 (68.3) | 69 (53.5) | — | — | — |
| Residence in a country with a higher average UV index than Latvia | |||||
| 20 (10.6) | 13 (65.0) | 0.213 | 1.835 | 0.698–4.827 | |
| More than two weeks per year relaxing in the sun (in comparison to “less”) | |||||
| 147 (77.4) | 83 (56.5) | 0.026* | 2.188 | 1.088–4.403 | |
| Sunbed use | |||||
| 11 (5.8) | 5 (45.5) | 0.662 | 0.762 | 0.224–2.587 | |
| Skin cancer history | |||||
| 24 (12.6) | 13 (54.2) | 0.786 | 1.126 | 0.477–2.658 | |
* Statistically significant.
Discussion
In this study we examined the prevalence of AK, individual and UV related risk factors and their associations in elderly population of Latvian. We found that more than a half (51.8 %) of individuals after the age of 60 had one or more AK, with greater prevalence in men (62.5 % vs. 47.4 %). This result is much higher than expected and estimated by the WHO (Lucas, 2006) but the fact that study population consisted of participants in a skin cancer screening campaign has to be taken in consideration. The recently reported prevalence of actinic keratoses in other European countries is lower – ranging from 49 % in men and 28.1 % in women in Rotterdam study (age from 51 year) to 16.36 % in men and 6.29 % in women in study on German employees (age group 61–70 years) (Flohil, 2013; Schaefer, 2014). The greater prevalence in men is in accordance with other studies (Traianou, 2012).
This study also indicates severe sunburns with blister formation or erythema lasting for more than two days in the age group of younger than 18 years old and those spending more than two weeks per year relaxing in the sun, which account as two major risk factors for AK development. It also shows that risk of AK increases with the increasing number of such sunburns. The association between sunburns in childhood and AK is in accordance with previous studies (Frost, 1998; Kennedy, 2003; Traianou, 2012). Spending more than two weeks per year relaxing in the sun is a marker of high cumulative UV exposure that is considered the primary cause of AK as absorption of both ultraviolet A and B radiation produces disruptions in intracellular signalling, cytokine regulation, and protective apoptotic mechanisms (Berman, 2013). At the same time other markers of high cumulative UV exposure are outdoor job and time spent in countries with high UV index, but this study did not show an association between those and prevalence of AK. It is in accordance with Rotterdam study that also found no such associations (apart from history of living in a sunny country for more than a year that had a protective effect on the development of 4 to 9 AK) (Flohil, 2013). At the same time in a study by Traianou et al., an outdoor occupation resulted in a fourfold increase of the risk for AK, and a residency in tropical countries resulted in more than threefold increase, if more than 10 years were spent (Traianou, 2012).
An association between skin type and presence of actinic keratoses was not found, although it has been shown in other studies (Traianou, 2012; Schaefer, 2014). The association was expected, but the difference might be explained by the fact that darker skin types (IV to VI) are rare and almost exclusively the first three phototypes are present in Latvian population and participants of this study.
This study also did not show an association between use of sunbeds and AK. Moreover, it showed that use of sunbeds is not prevalent among elderly population of Latvia and thus might not be a risk factor.
The results show that very few elderly people use sunscreens while being in the sun for more than an hour and even more surprising – while sunbathing. This together with the great prevalence of sunburns before the age of 18 suggests an inadequate protection from solar UV radiation and importance of information and education on sun-protection measures. The results from randomised controlled trials suggest that regular use of sunscreens prevents the development of AK and hastens the remission of existing lesions (Thompson, 1993; Werner, 2013; Iannacone, 2014). In this study sunscreen usage showed no protective effect on AK. Some other studies where sunscreen usage was low also did not show such effect (Naldi, 2006).
This study did not find an association between skin cancer history and presence of AK. Most of the cancers in patients’ histories were basal cell carcinomas (91.7 %), and other studies have found association (Naldi, 2006; Kaskel, 2015) and markedly higher risk of basal cell carcinomas in patients with AK (Khalesi, 2013). The reason why the association was expected is that ultraviolet radiation is the major etiologic agent in the pathogenesis of both basal cell carcinoma and actinic keratosis (Khalesi, 2013; Kennedy, 2003). Some of the reasons why the association was not found could be that patients with skin cancer history would most likely be interested in participation in a skin cancer screening campaign and that cancer history was asked in general without specifying the type, although several types of basal cell carcinoma are known and localisation.
This study has certain limitations. First, the population was not randomly selected. The screening was announced in mass media and everyone interested could participate and most often people with great amount of different skin lesions apply for such campaigns. Then, the majority of patients were female (70.7 % vs. 29.3 %), but the values are close to those provided by Central Statistical Bureau of Latvia on Latvian population distribution by age and gender – in year 2013, from total amount of permanent residents after the age of 60, 65.3 % were female and 34.7 % were male (Central Statistical Bureau of Latvia).
Conclusions
This study shows that the prevalence of actinic keratosis might be higher in Latvian population than previously expected. It also highlights severe sunburns before the age of 18 and more than two weeks per year spent relaxing in the sun as two most important risk factors for AK development. In relation to protection from UV radiation, this study indicates a very low sunscreen usage among elderly population of Latvia that might be one of the reasons for high prevalence of AK.
References
- Berker de D., McGregor J. M., Hughes B. R. Guidelines for the management of actinic keratosis. British Journal of Dermatology, 2007; 156: 222–230.
- Berman B., Cockerell C. J. Pathobiology of actinic keratosis: Ultraviolet-dependent keratinocyte proliferation. J Am Acad Dermatol, 2013; 68: S10-S19.
- Central Statistical Bureau of Latvia. Population by sex and age at the beginning of year. http://data.csb.gov.lv/pxweb/lv/Sociala/Sociala__ikgad__iedz__iedzskaits/IS0060.px/table/tableViewLayout1/?rxid=09cbdccf-2334-4466-bdf7-0051bad1decd (sk. 03.06.2015.).
- Ferrándiz C., Fonseca-Capdevila E., García-Diez A., et al. Spanish adaptation of the European Guidelines for the evaluation and treatment of actinic keratosis. Actas Dermosifiliogr, 2014; 105 (4): 378–393.
- Flohil S. C. van der Leest R. J. T., Dowlatshahi E. A., et al. Prevalence of actinic keratosis and its risk factors in the general population: The Rotterdam study. Journal of Investigative Dermatology, 2013; 133: 1971–1978.
- Frost C. A., Green A.C., Williams G.M. The prevalence and determinants of solar keratoses at a subtropical latitude (Queensland, Australia). British Journal of Dermatology, 1998; 139: 1033–1039.
- Iannacone M. R., Hughes M. C. B., Green A. C. Effects of sunscreen on skin cancer and photoaging. Photodermatol Photoimmunol Photomed, 2014; 30: 55–61.
- Kaskel P., Lange U., Sander S., et al. Ultraviolet exposure and risk of melanoma and basal cell carcinoma in Ulm and Dresden, Germany. JEADV, 2015 (29): 134–142.
- Kennedy C., Bajdik C. D., Willemze R., et al. The Influence of painful sunburns and lifetime sun exposure on the risk of actinic keratoses, seborrheic warts, melanocytic nevi, atypical nevi, and skin cancer. J Invest Dermatol, 2003; 120: 1087–1093.
- Khalesi M., Whiteman D. C., Doi S. A. R., et al. Cutaneous markers of photo-damage and risk of basal cell carcinoma of the skin: a meta-analysis. Cancer Epidemiol Biomarkers Prev, 2013; 22 (9): 1483–1489.
- Lucas R., McMichael T., Smith W., Armstrong B. Solar ultraviolet radiation: global burden of disease from solar ultraviolet radiation. Environmental Burden of Disease Series No. 13. Geneva (Switzerland): World Health Organization, 2006, 187.
- MacKie R. M. Awareness, knowledge and attitudes to basal cell carcinoma and actinic keratoses among the general public within Europe. J Eur Acad Dermatol Venereol, 2004; 18: 552–555.
- Naldi L., Chatenoud L., Piccitto R., et al. Prevalence of actinic keratoses and associated factors in a representative sample of the Italian adult population. Results from the prevalence of actinic keratoses Italian study, 2003–2004. Arch Dermatol, 2006; 142 (6): 722–726.
- Röwert-Huber J., Patel M. J., Forschner T., et al. Actinic keratosis is an early in situ squamous cell carcinoma: a proposal for reclassification. British Journal of Dermatology, 2007; 156 (3): 8–12.
- Rosen T., Lebwohl M. G. Prevalence and awareness of actinic keratosis: barriers and opportunities. J Am Acad Dermatol, 2013; 68: S2–9.
- Schaefer I., Augustin M., Spehr C., et al. Prevalence and risk factors of actinic keratoses in Germany – analysis of multisource data. Journal of the European Academy of Dermatology and Venereology, 2014; 28: 309–313.
- Thompson S. C, Jolley D., Marks R. Reduction of solar keratoses by regular sunscreen use. N Engl J Med, 1993; 329: 1147–1151.
- Traianou A., Ulrich M., Apalla Z., et al. Risk factors for actinic keratosis in eight European centres: a case–control study. British Journal of Dermatology, 2012; 167: 36–42.
- Werner R. N., Sammain A., Erdmann R., et al. The natural history of actinic keratosis: a systematic review. British Journal of Dermatology, 2013; 169: 502–518.
- Zalaudek I., Piana S., Moscarella E., et al. Morphologic grading and treatment of facial actinic keratosis. Clinics in Dermatology, 2014; 32: 80–87.



