Breast Cancer Patients Survival Rates at Pauls Stradiņš Clinical University Hospital
Abstract
Breast cancer is the most common malignant tumour in women in Latvia. The incidence of breast cancer increases gradually. Since 2006, each year in Latvia more than 1000 women are diagnosed with primary breast cancer. In 2010, breast cancer mortality rate per 100 000 women in Latvia was 23.7. Mortality rate per 100 000 women demonstrates the situation of breast cancer in the country, it describes disease long-term prognosis, risk factor influence on cancer development, and treatment possibilities.
The purpose of this study was to calculate breast cancer patients’ survival rates at Pauls Stradiņš Clinical University Hospital (PSCUH), depending on the disease onset, cancer morphological type and molecular subtype, and to compare the results with the survival rates in developed countries.
The retrospective study was performed for 377 breast cancer patients, who were treated at PSCUH during the period from 2005 to June 2010 (80% of all surgically treated breast cancer patients in the period). Patients’ data were collected from National Cancer Registry and Institute of Oncology databases. To calculate the relative 3- or 5-year survival rates, survived days from the day of diagnosis for each patient were performed separately. For statistical analysis Kaplan–Meier estimator and the ratio between number of survived patients and number of patients at the beginning of the study were used.
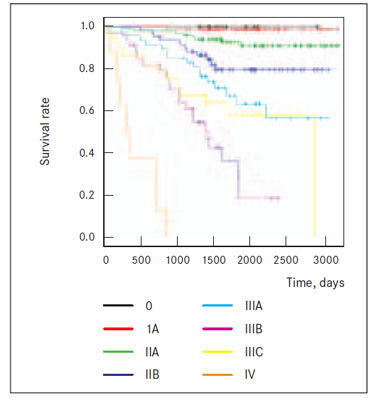
Breast cancer patients’ relative 5-year survival was 75.5 %. Relative 5-year survival rates, depending on the stage were as follows: stage 0 – 100 %; stage I – 98 %; stage II – 83 %, stage III – 47 %; stage IV – 0 %. 3-year survival rate for ductal and lobular cancer was 86.7% and 90%, respectively. Depending on molecular subtype, the highest 3-year survival rate has Luminal A cases (93.1 %), and the lowest rate has triple negative cases (77.1 %).
PSCUH breast cancer patients’ relative 5-year survival rate at stages I and II were comparable with the survival rates from Western countries, but stage III survival rate demonstrated a tendency to be slightly lower.
Introduction
Breast cancer is the most common cancer in women worldwide and the second most common cancer overall [2]. In 2012, nearly 1.7 million new breast cancer cases were diagnosed [2, 3]. In Europe, in 2012 there were around 470 000 new breast cancer cases [2]. The incidence of breast cancer varies greatly around the world. The highest age-standardised incidence rate for breast cancer in Europe in 2012 was in Belgium – 111.9 cases per 100 000 inhabitants, and the lowest incidence rate was in Bosnia Herzegovina with only 37.4 cases per 100 000 people [3].
In Latvia, breast cancer is the most common malignant tumour in women. In Latvia, since 2006, each year more than 1000 new cases are diagnosed. In 2013, 1133 women in Latvia were diagnosed with primary breast cancer, the age-standardised incidence rate for breast cancer was estimated to be 56.3 cases per 100 000 people. 2/1133 (0.2 %) cases were diagnosed in stage 0, 301/1133 (27 %) in stage I, 405/1133 (36 %) in stage II, 263/1133 (23 %) in stage III and 68/1133 (6 %) in stage IV. In 5 % of cases, the stage was not known and in 3% of cases cancer diagnosis was registered after death [3].
In 2010, breast cancer mortality rate per 100 000 women in Latvia was 23.7. Mortality rate of breast cancer in Latvia is higher compared to other European countries such as Spain, Portugal, Norway, Sweden, but lower if compared to Denmark [3, 4].
Aim
The main goal of this study was to analyse PSCUH breast cancer patients’ relative specific 5-year survival rate, depending on the stage of the disease, and relative specific 3-year survival rate, depending on the breast cancer morphological type, grade and molecular subtype, and to compare the results with the survival rates in Latvia on the whole as well as in developed countries.
Material and methods
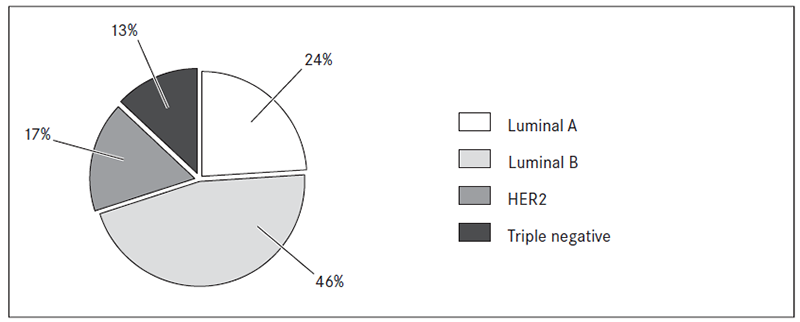
The retrospective study was performed for 377 breast cancer patients, who were treated in PSCUH during the period from 2005 to June 2010 (80 % of all breast cancer patients, who were treated in the Department of Surgery, PSCUH in the period). The patients’ data were collected from two databases – the National Cancer Register database and the Institute of Oncology database. Inclusion criteria were as follows: histologically confirmed breast cancer and survival data available. Distribution of patients according to the disease onset at the time of diagnosis has been represented in Table 1. In all cases, 7th edition of TNM classification was used. Distribution of patients according to histological type, grade and molecular subtype, if available, has been demonstrated in Figures 1, 2, 3.
The group of 377 patients was used to calculate the relative overall 3-year survival rate for all patients, who were treated in PSCUH in the period from 2005 to June 2010. For cases where respective data were available, breast cancer specific survival, depending on morphological type, grade, and molecular subtype were calculated. In our study we used following definitions for molecular subtypes of breast cancer: Luminal A type (positive oestrogen and/or progesterone receptors, HER2 receptor is negative, Ki67 < 14 %) Luminal B type (positive oestrogen and/or progesterone receptors and positive HER2 receptor, or Ki67 > 13 %), HER2 type (only HER2 receptor is positive), triple negative type (none of the receptors is positive) [1].
Table 1. Distribution of patients by stage (n = 377)
| Stage | Percentage | Number of patients, n |
|---|---|---|
| In situ | 3 | 11 |
| Stage I | 23 | 88 |
| Stage II | 42 | 161 |
| Stage IIA | — | 101 |
| Stage IIB | — | 60 |
| Stage III | 29 | 109 |
| Stage IIIA | — | 47 |
| Stage IIIB | — | 34 |
| Stage IIIC | — | 28 |
| Stage IV | 2 | 8 |
Group of 216 patients, who were treated in PSCUH in the period from 2005 to 2008, was used to calculate relative 5-year survival and breast cancer specific survival, depending on the onset of the disease.
To statistically calculate the relative 3- and 5-year survival, for each patient survived days from the day of diagnosis were calculated separately. Last update on status alive or dead was performed on 01.01.2014. For statistical analysis Kaplan–Meier estimator and the ratio between number of survived patients and the number of patients at the beginning of the study were used.
Figure 1. Distribution of patients by breast cancer morphological type (n = 377)
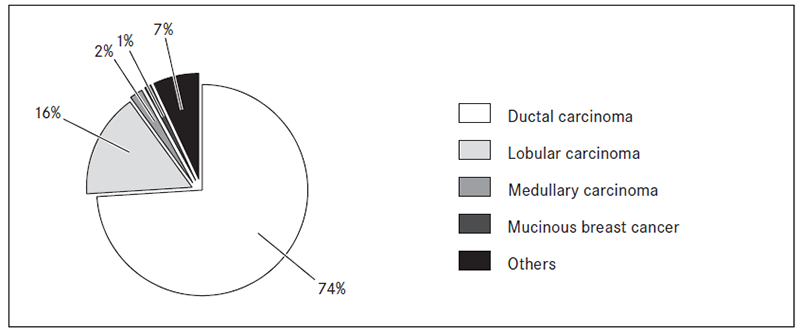
Figure 2. Distribution of ductal breast cancer patients by grade (n = 279)
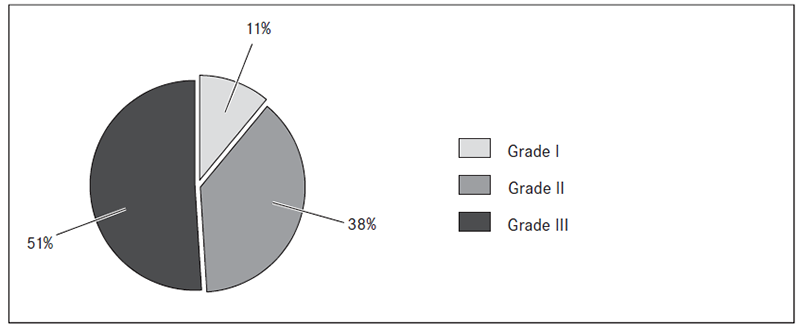
Figure 3. Distribution of patients by breast cancer molecular subtype (n = 362)
Results
From 377 patients, 77 died from breast cancer, during the study period. 48 out of 77 cases, died from the disease within 3 years from the time of diagnosis. Breast cancer specific 3-year survival for all stages is 87.3 % (Figure 4).
Analysing the group of 216 patients, who were treated in PSCUH in the period from 2005 to 2008, 53 cases of death from breast cancer were detected within 5 years from the time of diagnosis. Breast cancer specific 5-year survival is 75.5 % (Figure 5).
Data on breast cancer specific 5-year survival rate according to the stage of disease and respective USA and UK data can be seen in Table 2.
Figure 4. Distribution of 377 patients by disease status on 01.01.2014
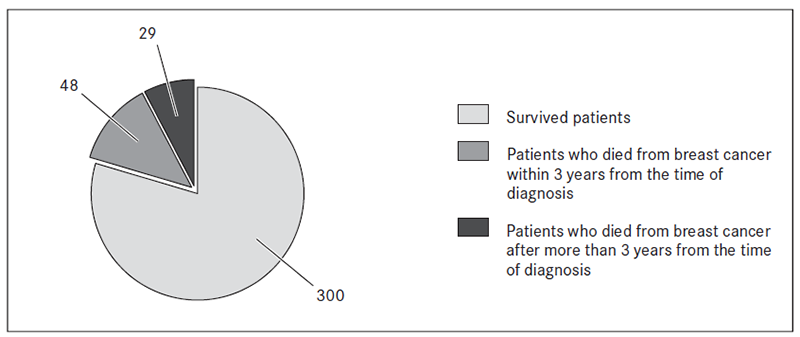
Figure 5. The distribution of 216 patients by disease status on 01.01.2014
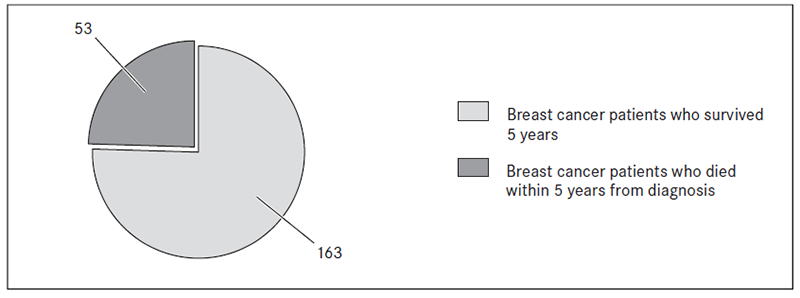
Table 2. 5-year survival rate of breast cancer patients, depending on the stage of the disease
| Stage | PSCUH* 5-year survival rate | 5-year survival rate in Latvia for breast cancer diagnosed in 2005 | 5-year survival rate in the USA (by NCI, 2012 data) [9] | 5-year survival rate in the UK (by cancer research, UK 2013) [8] |
|---|---|---|---|---|
| Stage 0 | 100 % | — | ~ 100 % | ~ 100 % |
| Stage I | 98 % | 88 % | ~ 100 % | > 90 % |
| Stage II | 83 % | 74 % | 85 % | > 70 % |
| Stage III | 47 % | 43 % | 66 % | > 50 % |
| Stage IV | 0 % | 4 % | 21 % | > 13 % |
* Pauls Stradiņš Clinical University Hospital.
The relative 3-year survival of ductal carcinoma (86.7 %) was slightly lower than relative 3-year survival of lobular carcinoma (90 %).
The breast cancer specific 3-year survival of ductal carcinoma according to grade was as follows: Grade I – 96.6 %; Grade II – 91 %; Grade III – 81 %.
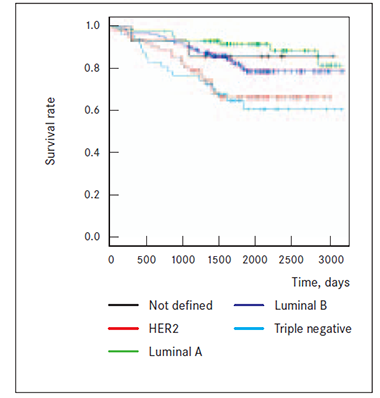
The breast cancer specific 3-year survival, depending on cancer molecular subtype is as follows: Luminal A type – 93 %; Luminal B type – 90 %; HER2 type – 79 %, triple negative type – 71 % (Figure 7).
Figure 6. Survival of breast cancer patients according | Figure 7. Survival of breast cancer patients, depending |
|---|---|
|  |
Discussion
According to National Cancer Registry (NCR) data, breast cancer 5-year survival for cases diagnosed in 2005 for all stages together is 61.7 %. This is considerably less than our PSCUH data – 75.5 %. However, we have to admit that in our study are included only the operated breast cancer cases and for stage IV the disease surgery is performed very rarely, mainly for hygienic reasons. Therefore, the proportion of stage IV cases in our study was only 2 %, but nationwide – 6 %. Metastatic breast cancer has poor prognosis and undoubtedly worsen overall 5-year survival, which is reported by NCR. Also higher rate of stage 0 (3 % vs. 0.2 %) and early stage (stage I and II) (65 % vs. 63 %) disease in our material comparing to NCR data could have some influence on better 5-year survival data.
We compared PSCUH data and nationwide 5-year survival data for breast cancer cases diagnosed in 2005 (see Table 2) according to the stage of disease. For stage I 5-year survival is 98 % and 88 %, for stage II – 83 % and 74 %, for stage III – 47 % and 43 % and for stage IV – 0 % and 4 %, respectively. The data show the tendency that 5-year survival for PSCUH cases in stages I–III is better than nationwide. One probable cause of such bias could be that nationwide data for breast cancer cases diagnosed in 2005 were used, but the study group also included cases diagnosed between 2005 and 2008. In 2006–2008, there was a comparably larger health care budget, which could have improved also the treatment results of breast cancer.
PSCUH data with 5-year survival data was also compared according to the stage of the disease from the USA and the UK. PSCUH stage 0–II data are very similar to the data from the USA reported by NCI as well as the UK data. We admit that number of stage 0 cases in our study is too small to draw any conclusions; however, it allowed detecting a tendency of 100% breast cancer specific 5-year survival, which is in accordance with natural course of non-invasive cancer. 5-year survival data for stage III disease in PSCUH and in Latvia altogether is rather similar. However, we detected that 5-year survival in stage III–IV cases is worse in PSCUH cases compared to the USA and the UK. Again, the number of stage IV disease in PSCUH material is too small for any conclusions, but the data by NCR show very clear difference between Latvia, the USA and the UK – 4 %, 21 % and > 13 %, respectively. There could be several possible explanations for poorer survival in stage III and IV breast cancer cases in PSCUH and Latvia treated in 2005–2008 including limited accessibility to cancer specialists, patients’ compliance and limited resources for breast cancer drugs.
The histopathological type and grade of the tumour have prognostic significance. Certain morphological types of breast cancer, such as medullary, mucinous and tubular have a more favourable long-term prognosis Our study did not show statistically significant difference of survival between the patients with diagnosed lobular breast carcinoma and patients with diagnosed ductal carcinoma, which is in concordance with the data of other authors [5, 7]. The 3-year survival rate correlated also with the tumour grade – the best for grade I cancers and the worst for grade III cancers, which is consistent with the data of other publications.
Breast cancer survival rate as well as long-term prognosis also depends on the cancer molecular subtype [5, 6]. Research showed that the highest survival rate was in patients with Luminal A molecular subtype. Patients with diagnosed Luminal B subtype, which was most common in our study, had lower survival compared to Luminal A, but overall had good long-term prognosis. On the other hand, patients with HER2 and triple negative molecular subtypes had much poorer long-term prognosis and significantly lower survival. Our results on survival in different breast cancer molecular subtypes confirm the earlier published data.
Conclusion
Breast cancer patients relative 5-year survival rate at stages I and II was comparable with the survival rates from developed countries, but at stages III and IV relative 5-year survival of breast cancer cases in Pauls Stradiņš Clinical University Hospital and Latvia showed a tendency to be worse. Those results may suggest, that treatment possibilities and patients’ compliance for advanced breast cancer cases (stages III and IV) in 2005 probably were worse, compared to the United Kingdom and the USA.
References
- Susan G. Komen website. Molecular subtypes of breast cancer. // http://ww5.komen.org/BreastCancer/SubtypesofBreastCancer.html (accessed on 02.05.2014).
- Cancer research UK charity website. Breast cancer incidence statistics // http://www.cancerresearchuk.org/cancerinfo/cancerstats/types/breast/incidence/uk-breast-cancer-incidence-statistics#source33 (accessed on 16.04.2014).
- World Health Organization. International Agency for Research on Cancer. GLOBOCAN 2012. Estimated cancer incidence, mortality and prevalence worldwide in 2012 // http://globocan.iarc.fr/Pages/fact_sheets_cancer.aspx
- Eurostat Home. European Commission statistics. Causes of death – standardised death rate // http://epp.eurostat.ec.europa.eu/statistics_explained/index.php?title=File:Causes_of_death_-_standardised_death_rate,_2010_%281%29_%28per_100_000_inhabitants%29.png&filetimestamp=20121022145128
- Bland K. I., Copeland E. M. (eds.) – The breast: Comprehensive management of benign and malignant diseases. – 4th ed. – Philadelphia, 2009. – Pp. 455–462.
- European Society for Medical Oncology. Molecular subtype of a breast cancer relapse influences patient post-relapse survival // http://www.esmo.org/Conferences/IMPAKT-2014-Breast-Cancer/News/Molecular-Subtype-of-a-Breast-Cancer-Relapse-Influences-Patient-Post-Relapse-Survival
- National Center for Biotechnology Information. Prognostic value of histologic grade nuclear components of Scarff–Bloom–Richardson // http://www.ncbi.nlm.nih.gov/pubmed/2551477?dopt=Abstract
- Cancer research UK charity website. Statistics and outlook for breast cancer // http://www.cancerresearchuk.org/cancer-help/type/breast-cancer/treatment/statistics-and-outlook-for-breast-cancer
- Fletcher Allen Health Care, Vermont University Hospital. Breast cancer treatment survival statistics // http://www.fletcherallen.org/about/health_report_cards/quality_of_care_reports/cancer_care/breast_cancer_treatment_survival_statistics.html