Childhood Intussusception: 10-year Experience at Children’s Clinical University Hospital in Riga
Abstract
Intussusception is the most common cause of intestinal obstruction in children between the age of 3 months and 3 years. Non-surgical methods are the main treatment, but still intussusception reduction techniques remain varied and controversial.
The aim of the study was to review the experience of Children’s Clinical University Hospital in the management of intussusception over the last 10 years, with a focus on assessing the efficacy of nonoperative reduction.
Retrospective descriptive study was conducted at Children’s Clinical University Hospital, Riga. The study included data from medical records of patients with intussusception between January 2006 and December 2015 at the hospital. Patients’ demographics, clinical presentation, treatment modalities, recurrence and length of hospital stay were studied. The method of non-operative reduction was pneumatic reduction. Data analysis was carried out using the Microsoft Excel and IBM SPSS Statistics. Results were considered statistically significant with CI > 95 %, p < 0.05.
The study included 148 patients (93 males, 55 females), ratio 1.7 : 1. Mean age 23.7 ± 27.4 months (range 2 to 161 month). Duration of presenting symptoms 18 ± 17 h, most common symptom – abdominal pain (83.1 %). Main diagnostic method – abdominal sonography, made in 81.1 %, with sensitivity of 95.8 %. Secondary intussusception found in 4.7 % with Meckel’s diverticulum (n = 5) and polyp (n = 2) as lead point. Pneumatic reduction was performed in 85 patients, with success rate of 82.5 %. In surgical group (n = 61) predominantly laparotomy with manual reduction in 24.3 % was used. The overall recurrence rate was 6.8 %. Mean hospital stay was 4.6 days, in non-surgical group 2.5 days vs. surgical group 7.5 days (p < 0.01).
Pneumatic reduction is the main intussusception treatment method at Children’s Clinical University Hospital. There is no statistically significant correlation between patient’s age, length of symptoms and pneumatic reduction success rate. Pneumatic reduction is minimally invasive for patients, has high success rate (82.5 %) and low complication rate, decreases length of hospital stay.
Introduction
Intussusception is the most common cause of intestinal obstruction in infants and young children between the age of 3 months and 3 years, and the peak age of presentation is 4 to 10 months [7, 508; 14, 518]. It is acquired invagination of one portion of the intestine into the adjacent bowel and described by the proximal, inner segment of intestine first and the outer distal, receiving portion of intestine last [7, 508]. Intussusception results in venous congestion and bowel wall oedema, and if left untreated, arterial obstruction, bowel necrosis and perforation may occur [14, 518]. 80 % to 95 % of paediatric intussusceptions are ileocolic and idiopathic, mostly caused by lymphoid hyperplasia as the “lead point” in its pathogenesis [14, 519]. Secondary intussusception is observed in 1.5 % to 12 % of cases, on average 6 % [5, 141; 8, 509; 14, 519]. The most common causes are Meckel’s diverticulum, polyps and duplications. Systemic conditions such as Henoch-Schönlein purpura, Peutz-Jeghers syndrome can also increase the risk of intussusception [14, 519]. Secondary intussusception proportion increases with age, particularly after 2 years of age [7, 515].
Techniques for intussusception reduction remain varied and controversial. Treatment may be nonsurgical (pneumatic or hydrostatic pressure enemas under fluoroscopy or sonography) or surgical (laparoscopy, open surgery with manual reduction and/or resection or enterostomy) [3, 4; 7, 511; 12, 60; 14, 522].
Hydrostatic reduction was first described in 1876. Barium or water-soluble contrast enema are used for hydrostatic reduction under fluoroscopy, with no more than three attempts, no more than three minutes each. Hydrostatic reduction is complete when contrast medium freely flows through the ileocecal valve into terminal ileum. Success rate ranges between 42 % and 95 % [7, 519].
Air reduction was first described in 1897. It is being advocated as faster, safer, much leaner method with less exposure time to radiation. The maximum safe air pressure is 80 mmHg for younger infants and 120 mmHg for older ones [7, 520]. Pneumatic reduction is currently the most popular standard method with success rate of 84 % to 100 % [12, 60; 14, 522]. Disadvantages of fluoroscopic reduction methods are related to exposure to radiation, poor visualisation of lead points, relatively poor visualisation of reduction process, resulting in false-positive reduction. Complications as bowel perforation, barium peritonitis, tension pneumoperitoneum, fewer and septicaemia are described [7, 520; 8, 1138].
Sonographically guided hydrostatic intussusception reduction was first described in 1985 [12, 59]. Reduction can be done without general anaesthesia. The enema bag is raised initially to three feet and subsequently elevated to a maximum of 5.5 feet if reduction is not achieved after two attempts. A successful reduction is confirmed when the entire caecum and thickened ileocaecal valve are visualised with free flow of fluid into the distal small bowel [12, 60]. Advantages of such method are excluding the need of radiation, possibility for parents to take part in treatment process, significantly higher sensitivity in detecting pathologic lead points, and earlier evaluation for bowel perforation signs. The major disadvantage, however, is the need in sonographic experience in intussusception diagnostic and reduction evaluation [12, 63].
Operative reduction is required when non-operative reduction is either contra-indicated (peritonitis, perforation) or unsuccessful [14, 519]. At this moment, there are no approved guidelines for intussusception treatment.
Aim
The goal of this study is to review the experience of Children’s Clinical University Hospital in the management of paediatric intussusception over the last 10 years, with a focus on assessing the efficacy of non-operative reduction.
Material and Methods
This is a retrospective descriptive study conducted at Children’s Clinical University Hospital (CCUH) of Riga. Children who presented with intussusception between January 2006 and December 2015 at CCUH were included in the study. Data were extracted from medical records. Patients demographics, clinical presentation, duration of symptoms, treatment modalities, complication rate, and length of hospital stay were studied. Indications for non-surgical treatment for patients with intussusception before 2009 were age till 12 months, length of symptoms till 24 hours, no signs of ileus on abdominal plain x-ray, no massive bleeding from gastrointestial tract, no signs of peritonitis. After 2009, indications were changed to length of symptoms till 36 hours and age till 24 months, other indications remained the same.
The method of non-operative reduction in our institution was pneumatic reduction under fluoroscopy. The procedure was performed by paediatric surgeon. During pneumatic reduction, air is insufflated via Foley catheter (size of 18-Fr to 22-Fr, depending on a patient’s size, with balloon inflated with 10 ml of water) placed inside a patient’s rectum under pressure monitoring with a maximum of 120 mmHg. Manipulation was made under general anaesthesia. Successful reduction was demonstrated by free flow of air into terminal ileum and disappearance of caecal soft tissue mass. In surgical reduction both methods, laparoscopy and laparotomy, were used.
Data analysis was carried out using the Microsoft Excel and IBM SPSS Statistics. Results were considered statistically significant when p ≤ 0.05.
Results
Between January 2006 and December 2015, 148 patients (94 male, 54 female) with intussusception were admitted to CCUH. Intussusception was diagnosed more often in males than in females, male to female ratio was 1.7 : 1. Number of cases increased in last years (Figure 1), that can be explained with the increasing number of cases transmitted from regional hospitals to Children’s Clinical University Hospital of Riga.
Mean age at presentation was 23.7 ± 27.4 months (range 2 to 161 months). More than half of the patients (50.7 %) presented were at the age before one, 28.4 % in the age group 1 to 3 year-olds and 20.9 % older than 3 years (Figure 2). Duration of presenting symptoms was 18 ± 17 hours (range 1 to 72 hours). Distribution of the patients in relation to the duration of symptoms is presented in Table 1. The most common symptom reported was intermittent crampy abdominal pain, found in 123 (83.1 %) patients. Classic clinical triad (intermittent, crampy abdominal pain, “red currant jelly” stool, vomiting) was reported only in 26.4 % (39) patients. Presence of palpable abdominal mass was not described in medical literature. Common presenting symptoms are represented in Table 2.
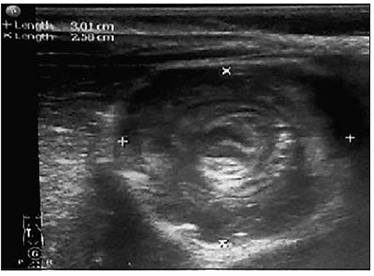
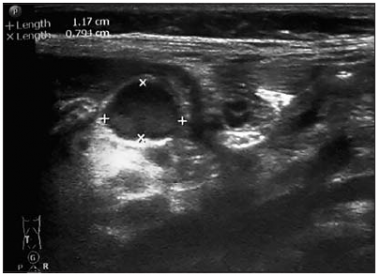
Main diagnostic methods used at Children’s Clinical University Hospital were abdominal sonography and plain abdominal X-ray. Computer tomography for intussusception confirmation was used only once in a 10-year period. Abdominal sonography was made in 81.1 % (120) patients with sensitivity of 95.8 % (Figure 3). Possible pathologic lead point was found in 41.7 % (50) of cases (Figure 4). In recent years sonography use in control for early recurrence has increased, made in 55 (37.2 %) patients, revealed 12 (8.1 %) recurrence cases. Plain abdominal X-ray was made in 66.9 % (99) patients, ileus signs were found in 58.6 % (58), irregular distribution of gases in 29.3 % (29) and normal – in 12.1 % (12) cases.
Figure 1. Distribution of patients with intussusception per year
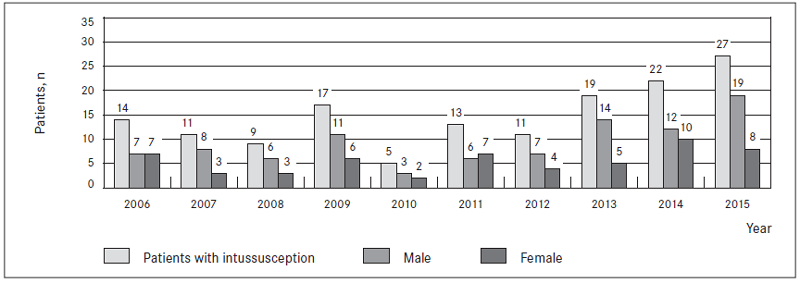
Figure 2. Frequency of intussusceptions in different age groups and sexes
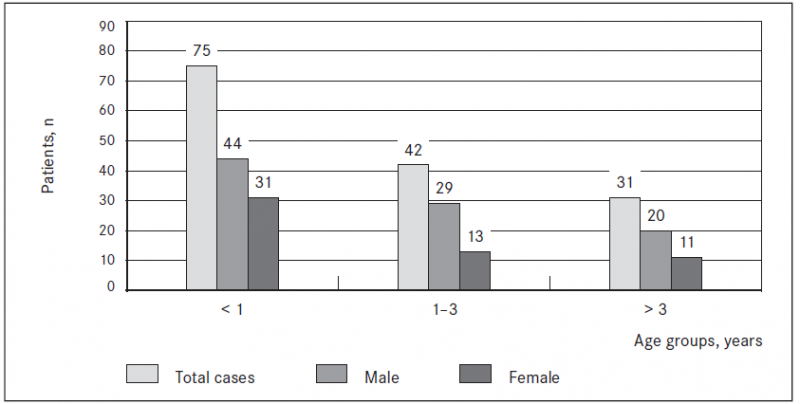
Table 1. Distribution of patients in relation to the duration of symptoms
| Duration of symptoms, h | Number of patients, n (%) | Successful non-operative reduction, % |
|---|---|---|
| < 24 | 111 (75) | 62.2 |
| 24–48 | 30 (20.3) | 46.7 |
| > 48 | 7 (4.7) | 28.6 |
Table 2. Distribution of intussusception symptoms
| Presenting symptom | Number of patients, n (%) |
|---|---|
| Abdominal pain | 123 (83.1) |
| Vomiting | 109 (73.6) |
| Red currant jelly stool | 64 (43.2) |
| Lethargy | 42 (28.4) |
| Irritability | 43 (29.1) |
Figure 3. Intussusception sonographic view – target sign (examination and image made by K. Soldatenkova) | Figure 4. Mesenterial lymphadenitis sonographic view (examination and image made by K. Soldatenkova) |
|
|
Pneumatic reduction was performed in 103 patients, among which 85 (82.5 %) cases were successful, no bowel perforation was observed after procedure. In total, 57.4 % of patients were treated with pneumatic reduction. No statistically significant correlation between pneumatic reduction success rate and patient’s age, length of symptoms was found (Table 3).
Table 3. Pneumatic reduction success rate in correlation to age and symptoms length
| Criterion | Number of patients | Pneumatic reduction attempt | Successful pneumatic reduction | Success rate, % | p value | |||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |||
| All patients | 148 | 100.0 | 103 | 69.5 | 85 | 57.4 | 82.5 | |
| < 1 year | 75 | 51.0 | 55 | 73.3 | 43 | 57.3 | 78.2 | 0.997 |
| 1–3 years | 42 | 28.0 | 27 | 64.3 | 24 | 57.1 | 88.9 | |
| > 3 years | 31 | 21.0 | 21 | 67.7 | 18 | 58.1 | 85.7 | |
| Symptoms < 24 h | 111 | 76.7 | 86 | 77.5 | 69 | 62.2 | 80.2 | 0.090 |
| Symptoms 24–48 h | 30 | 20.3 | 15 | 50.0 | 14 | 46.7 | 93.3 | |
| Symptoms > 48 h | 7 | 4.7 | 2 | 28.6 | 2 | 28.6 | 100.0 | |
A total of 61 patients in the study required operative reduction (Figure 5). The most frequently performed was laparotomy with manual reduction in 36 (24.3 %) patients, laparotomy with bowel resection and primary bowel anastomosis in 5 (3.4 %), laparotomy with bowel resection and stoma in 2 (1.4 %) patients. Laparoscopic reduction was attempted in 25 patients, among whom 18 (12.2 %) were successful. Conversion to open reduction was required in five patients due to difficult reduction, and in one because of the need for bowel resection. In one case laparoscopy was made as diagnostic operation after spontaneous intussusception reduction and persistent clinical symptoms, but no intussusception was found during the operation. Together in two (1.4 %) patients with clinically and sonographically confirmed intussusception after observation period under sonogaphy control spontaneous reduction was diagnosed without a need for further non-surgical or surgical treatment. Comparison of pneumatic reduction group and surgical reduction group is shown in Table 4.
In our study 136 (91.9 %) patients were with intussusception at the hepatic flexure (ileocolic), 82 (60.3 %) of whom had successful non-operative reduction; other forms of intussusception were less common (Table 5).
Figure 5. Treatment methods for patients with intussusception
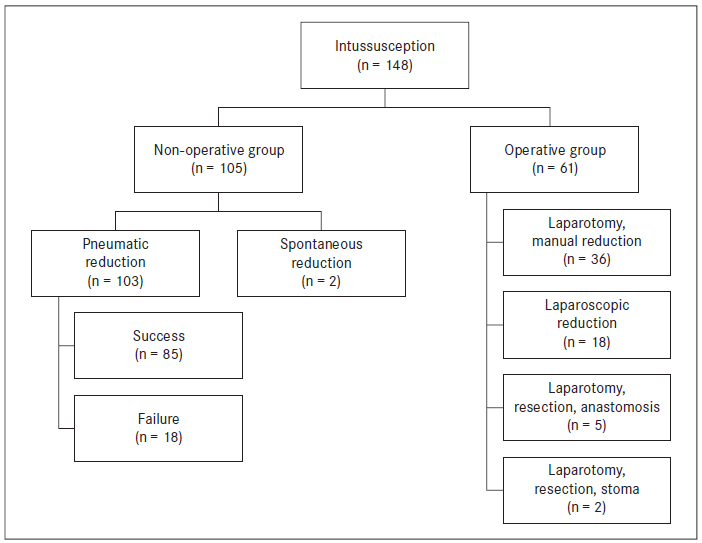
Table 4. Comparison of pneumatic reduction and operative reduction groups
| Criterion | Pneumatic reduction group (n = 85) | Operative reduction group (n = 61) | p value |
|---|---|---|---|
| Gender, n (%) | Male 48 (56.5) | Male 44 (72.1) | 0.053 |
| Female 37 (43.5) | Female 17 (27.9) | ||
| Age, month (mean) | 21.9 ± 22.6 | 24.0 ± 28.3 | 0.619 |
| Age groups, n (%) | |||
| < 1 year | 43 (57.3) | 32 (42.7) | 0.968 |
| 1–3 years | 24 (58.5) | 17 (41.5) | |
| > 3 years | 18 (60.0) | 12 (40.0) | |
| Length of symptoms, h (mean) | 15.5 ± 15.3 | 22.6 ± 18.9 | 0.013 |
| Length of symptoms, n (%) | |||
| < 24 h | 69 (63.3) | 40 (36.7) | 0.069 |
| 24–48 h | 14 (46.7) | 16 (53.3) | |
| > 48 h | 2 (28.6) | 5 (71.4) | |
| Symptoms, n (%) | |||
| Intermittent pain | 68 (80.0) | 53 (86.9) | 0.276 |
| Vomiting | 58 (68.2) | 49 (80.3) | 0.103 |
| Red currant jelly stool | 30 (35.3) | 34 (55.7) | 0.014 |
| Plain abdominal X-ray, ileus | 30 (52.6) | 28 (66.7) | 0.324 |
| Intussusception type, n (%) | |||
| Idiopathic | 84 (98.9) | 55 (90.2) | 0.051 |
| Secondary | 1 (1.1) | 6 (9.8) | |
| Length of hospital stay, days (mean) | 2.5 ± 1.9 | 7.5 ± 3.8 | < 0.001 |
Table 5. Distribution of intussusception forms in relation to the treatment method
| Intussusception form | Pneumatic reduction cases, n | Operative reduction cases, n | Spontaneous reduction, n | Total, n (%) |
|---|---|---|---|---|
| Ileocolic | 82 | 52 | 2 | 136 (91.9) |
| Ileoileocolic | 0 | 2 | 0 | 2 (1.4) |
| Ileoileal | 3 | 4 | 0 | 7 (4.7) |
| Colocolic | 0 | 2 | 0 | 2 (1.4) |
| Appendicocaecal | 0 | 1 | 0 | 1 (0.7) |
A pathological lead point was noted in 86 (58.1 %) patients, with prevalence of acute mesenterial lymphadenitis in 79 (91.9 %) patients as primary or idiopathic intussusception possible reason. The cause for secondary intussusception was found in 7 (4.7 %) patients. Five cases of Meckel’s diverticulum and two cases of bowel polyps were found. One patient was admitted to Children’s Clinical University Hospital with intussusception after Rota virus vaccine in close history. Distribution of patients with pathological lead point are presented in Table 6. Pathological cause was found in 10 of 18 unsuccessful pneumatic reduction cases: two cases of Meckel’s diverticulum, eight cases of acute mesenteric lymphadenitis.
Recurrence was divided in two groups. Early recurrence during same hospitalisation in first 24–72 hours after non-surgical or surgical treatment. Together 12 (8.1 %) cases were included, seven cases after surgical and five cases after non-surgical treatment. Distribution of used treatment methods is shown in Table 7. Ten from 148 children had more than one episode between 2006 and 2015, overall recurrence rate was 6.8 % (10/148). Number of recurrence episodes ranged from one to four times. Higher number occurred in males with Meckel’s diverticulum. Only in two patients it was possible to identify pathological lead factor (Meckel’s diverticulum and bowel polyp). The period of intussusception recurrence onset ranged from 1 month to 4.8 years.
Mean post reduction hospital stay was 4.6 days (range, 1–18 days). In pneumatic reduction group mean hospital stay was 2.5 days (range, 1–7 days) versus 7.5 days (range, 3–17 days) in surgical group: laparoscopy – 5.6 days, laparotomy with manual reduction – 7.6 days. There was a statistically significant difference in length of hospital stay between non-operative and operative groups (p < 0.001).
Table 6. Distribution of patients with pathological lead point in relation to age
| Age (years) | Number of patients, n (%) | Number of patients with pathological lead point, n (%) | Idiopathic intussusception, n | Secondary intussusception, n |
|---|---|---|---|---|
| < 1 | 75 (51) | 30 (40.0) | 24 | 6 |
| 1–3 | 42 (28) | 29 (69.0) | 29 | 0 |
| > 3 | 31 (21) | 27 (87.1) | 26 | 1 |
| Total | 148 (100) | 86 (58.1) | 79 | 7 |
Table 7. Patients with recurrent intussusception treatment methods
| Treatment method | Number of patients, n |
|---|---|
| Pneumatic reduction | 2 |
| Laparotomy, manual reduction | 3 |
| Laparoscopic reduction | 2 |
| Laparotomy, resection, stoma | 2 |
| Spontaneous reduction | 3 |
| Total | 12 |
Discussion
Intussusception is the most common cause of intestine obstruction in infants and children between the age of 3 months and 3 years, and the peak age of presentation is 4 to 10 months [6, 23; 7, 508; 14, 518]. If diagnosed early, intussusception may be easily treated by non-surgical methods. For a successful management of intussusception, it is important to recognise pattern, risk factors, diagnostic and treatment methods [3, 1; 5, 139]. This study is the first retrospective analysis of Children’s Clinical University Hospital’s 10-year experience.
The study included 148 patients, with mean age of 23.7 months (range, 2–161, median 13 months), more than a half (50.7 %) below the age of one. Statistically significant prevalence in males with ratio 1.7 : 1. Median age in our study is higher to the data from the analysed literature, with median age 7–19 months [3, 2; 8, 1839; 11, 217], but agrees with male : female ratio 1.3–2 : 1 [3, 2; 8, 1840; 11, 218].
Typical intussusception symptoms or “clinic triad” include crampy, intermittent pain, red currant jelly stool and vomiting [5, 140] or abdominal mass [14, 519] is seen in less than 25 % of patients. The leading symptom also varies according to publications, Wong et al. described vomiting as leading symptoms (76.3 % of patients) [14, 520], but Guney et al. found abdominal pain in all patients [5, 140]. Red currant jelly stool was observed in 12.4–71.5 % of patients [5, 140; 8, 1839]. Various studies [8, 1840; 10, 843; 14, 520] have reported palpable abdominal mass as statistically significant risk factor for unsuccessful non-operative reduction, because this may signify relatively longer duration of intussusception, complete intestinal obstruction. In our study “classic triad” (pain, vomiting, red currant jelly stool) was found in 26.4 % of cases, with intermittent abdominal pain as the leading symptom in 83.1 % of cases, consistent with literature. Palpable abdominal mass was not evaluated due to lack of information in medical records.
Sonography has become the diagnostic standard for confirmation of suspected intussusception, with high sensitivity (98–100 %) and specificity (88–100 %), [5, 139; 12, 59; 14, 519] especially in ileocolic intussusception form [2]. In our study abdominal sonography was performed in 81.1 % of patients, with sensitivity of 95.8 %. Abdominal radiography is the second diagnostic method used in the study – 99 cases (66.9 %), no cases of perforation detected. Tareen et al. analysed a 15-year experience in necessity of abdominal radiography (AR) in children with intussusception. They concluded that AR should always be performed when clinical peritonitis is present, but is not otherwise necessary in children with suspected or confirmed intussusception [13, 90].
The vast majority of patients with intussusception does not have a pathologic lead point and is classified as primary or idiopathic intussusception [8, 508]. In idiopathic intussusception, the most common cause is mesenterial lymphadenitis [1, 648; 8, 509; 14, 520]. Secondary intussusception with identifiable cause range from 1.5 % to 12 %. Most common found pathologies are Meckel’s diverticulum, polyps, duplications [5, 141; 8, 509; 14, 519]. These anatomic causes tend to increase in proportion by age, especially after 2 years of age [8, 509], in some studies after 4–5 years of age [1, 648]. The current study showed secondary intussusception in 4.7 %. Various studies have reported anatomical lead point as statistically significant risk factor for unsuccessful non-operative treatment [5, 141; 14, 520], especially in correlation with age after 2 years of age, anamnesis over 48 hours [8, 1841; 12, 60] and palpable abdominal mass [3, 2; 14, 520].
Intussusception reducing techniques remain varied and controversial, there are no guidelines found in literature [12, 59]. The two main directions are isolated: non-surgical and surgical. All analysed publications advocate non-surgical methods as main intussusception treatment methods, but no unified opinion can be found about such methods’ subtypes, contraindications, attempts’ number and specialist (surgeon vs. radiologist) who perform this manipulation [8, 1838; 12, 60]. At present, pneumatic reduction under fluoroscopy is the most popular method and is being advocated as a cleaner and faster technique, with high success rate 75–100 % [3, 2; 12, 60; 14, 520]. Sanchez et al. in retrospective analysis reviewed 31 cases of intussusception and compared sonographically guided hydrostatic saline enema reduction with pneumo and hydroreduction under fluoroscopy. Analysis showed success rate for sonographically and fluoroscopically assisted reduction 100 % and 84 %, respectively. The advantage of sonography compared to fluoroscopy is no concern over excessive radiation exposure, evaluation of possible pathologic lead points, greater sensitivity in visualising small fluid collections for diagnosis of possible perforation [12, 61]. In contrast, Khorana et al. compared 190 cases of intussusceptions, solved by pneumatic and hydrostatic reduction methods, guided under sonography and fluoroscopy. They found success rate of pneumatic and hydrostatic reduction 61 % and 26 %, respectively [8, 1841]. Lautz et al. in their study compared delayed repeat enema with immediate surgery in children with ileocolic intussusception and statistically proved that delayed repeat enemas are safe, increase success of non-operative reduction, decrease rate of bowel resection and reduce mean hospital length of stay and costs [9, 425]. Geltzeiler et al. report about laparoscopy – assisted hydrostatic reduction of intussusception in cases of failed reduction by contrast enema under fluoroscopy as treatment modality [4, 764]. In this study, pneumatic reduction under fluoroscopy was performed in 85 (57.4 %) patients with success rate of 82.5 %, which coincide with other authors’ results. Most reviewed studies as absolute contraindications for nonsurgical treatment mention only signs of peritonitis and bowel perforation, compared with the hospital’s contraindications of age, length of symptoms, ileus at X-ray [7, 509; 8, 1838; 14, 519].
Recurrence rate of intussusception varies from 3–20 %, with higher incidence in non-operative treatment group (3–15 %) and less than 5–8 % in operative group [3, 2; 7, 515]. Recurrence risk according to literature increase in first 24–48 hours after treatment episode and after 6 months [3, 3; 7, 515]. In the study, early recurrence was higher in non-operative group, but overall recurrence was 6.8 %, which corresponds to other reports.
Conclusions
- Pneumatic reduction is the main intussusception treatment method at Children’s Clinical University Hospital.
- There is no statistically significant correlation between patient’s age, length of symptoms and pneumatic reduction success rate.
- Pneumatic reduction is minimally invasive for patients, has high success rate (82.5 %) and low complication rate, decrease length of hospital stay.
References
- Banapour, P., Sydorak, R. M., Shaul, D. Surgical approach to intussusception in older children: influence of lead points. J Pediatr Surg. 2015, 50 (4): 647–650.
- Blanco, F. C., Cuffari, C., Wilkes, G., et al. Intussusception. Available from: http://emedicine.medscape.com/article/930708-overview (22.06.2016).
- Esmaeili-Dooki, M. R., Moslemi, L., Hadipo, A., et al. Pediatric intussusception in Northern Iran: comparison of recurrent with non-recurrent cases. Iran J Pediatric. 2016, 26 (2): 1–5.
- Geltzeiler, C. B., Sims, T. L., Zigman, A. F. LAHRI: laparoscopic-assisted hydrostatic reduction of intussusception. J Laparoendosc Adv Surg Tech A. 2015, 25 (9): 763–766.
- Güney, L. H., Fakioğlu, E., Acer, T., et al. Is every intussusception treatment an emergency intervention or surgery? Ulus Travma Acil Cerrahi Derg. 2016, 22 (2): 139–144.
- Huppertz, H. I., Soriano-Gabarro, M., Grimprel, E., et al. Intussusception among young children in Europe. Pediatr Infect Dis J. 2006, 25 (1): 22–29.
- Ignacio, R. C., Fallat, M. E. Intussusception. Ashcraft’s Pediatric Surgery. Ed. by Holcomb III, G. W., Murphy, J. P. 5th ed. Philadelphia: W. B. Saunders, 2010, 516–524.
- Khorana, J., Sihghavejsakul, J., Ukarapol, N., et al. Enema reduction of intussusception: the success rate of hydrostatic and pneumatic reduction. Therapeutics and Clinical Risk Management. 2015, 11: 1837–1842.
- Lautz, T. B., Thurm, C. W., Rothstein, D. H. Delayed repeat enemas are safe and cost-effective in the management of pediatric intussusception. J Pediatr Surg. 2015, 50 (3): 423–427.
- Mandeville, K., Chien, M., Willyerd, F. A., et al. Intussusception: clinical presentations and imaging characteristics. Pediatr Emerg Care. 2012. 28: 842–844.
- Ogundoyin, O. O., Olulana, D. I., Lawal, T. A. Childhood intussusception: a prospective study of management trand in a developing country. Afr J Paediatric Surg. 2015, 12 (4): 217–220.
- Sanchez, T. R., Doskocil, B., Stein-Wexler, R. Nonsurgical management of childhood intussusception. J Ultrasound Med. 2015, 34: 59–63.
- Tareen, F., McLaughlin, D., Cianci, F., et al. Abdominal radiography is not necessary in children with intussusception. Pediatr Surg Int. 2016, 32 (1): 89–92.
- Wong, C. W., Chan, I. H., Chung, P. H., et al. Childhood intussusception: 17-year experience at a tertiary referral centre in Hong Kong. Hong Kong Med J. 2015, 21 (6): 518–523.