Mandibular Condyle Characteristics in Juvenile Idiopathic Arthritis Patients Compared with Control Group by Cone Beam Computed Tomography Assessment
Abstract
Juvenile idiopathic arthritis (JIA) patients have a high risk of mandibular condyles being affected. Cone beam computed tomography (CBCT) has the advantage of providing 3D images allowing an accurate description of mandibular condyle features, morphology and disorders. Assessment of mandibular condyle structure in JIA patients using CBCT enables an understanding of the typical radiologic characteristics of morphological change in these JIA patients.
The aim of this study was to evaluate the mandibular condyle characteristics seen in CBCT and to compare them with the features observed in the control group of the same age.
A cross-sectional study analysing CBCTs of 65 (130 joints) patients with a confirmed JIA diagnosis and 30 (60 joints) control group – patients without JIA up to the age of 17. For the control group the inclusion criteria was an age of up to 17 years with an indication for CBCT scans such as impacted canines. Structural radiologic characteristics of the joint’s osseous structures were assessed in the sagittal, coronal and axial planes.
The flattening of the condyles was significantly more often seen in JIA patients compared to the controls (82.8 %) and more in females than in males. The surface erosion was seen only in the JIA group and affected 58.7 % and 63.0 % of the right and left side respectively in females. The osteophytes were a less frequently seen destruction characteristic and affected 39.1 % and 30.4 % of the right and left side respectively in JIA patients only.
Mandibular condyle destruction characteristics observed in CBCT images were frequent in the JIA group and occurred with less frequency in the control group.
Introduction
Temporomandibular joint (TMJ) condyles are frequently affected in juvenile idiopathic arthritis (JIA) and lesions in or on the condyles appear early in life of a patient below the age of 16 [Cassidy, 1986]. Females are more often affected than males [Ferraz et al., 2012] and can be affected uni- or bilaterally [Te Veldhuis et al., 2014]. Despite how minimal the damage to the condyle is, craniofacial morphology may become severely disturbed [Billiau et al., 2007]. The consequence of this inflammation and subsequent destruction during growth has a large variation in severity ranging from minor mandibular asymmetries with no clinical significance to major growth deviations of the mandible leading to disturbed mandibular function and growth [Billiau et al., 2007; Ringold et al., 2009; Arvidsson et al., 2010; Fjeld et al., 2010].
Detecting these destructive signs early in the course of the disease clinically and radiographically is critical. Early diagnosis of the disease and being aware of the potential outcomes of the disease on the condyles facilitates the formulation of a treatment plan compensating for possible future condylar destruction, hence decreasing the impact on mandibular growth and facial appearance [Twilt et al., 2004; Pedersen et al., 2008]. Diagnosis of TMJ arthritis includes clinical examination and imaging of the joint [Müller et al., 2009].
Conventional radiographic methods can only show gross osseous changes [Cassidy, 1986] and panoramic radiology is inadequate in identifying small osseous lesions on the surface of the condyle [Dahlstrom et al., 1996; Petersson et al., 2010]. The advantage of using cone beam computed tomography (CBCT) is the possibility for acquiring 3D images, which enable an accurate description of the underlying osseous structure, morphology and disorders of the TMJ whilst having a significantly lower radiation dose than conventional computer tomography [Swennen et al., 2006; Alexiou et al., 2009; Garagiola et al., 2013]. Magnetic resonance imaging (MRI) is still the gold standard for diagnosing TMJ arthritis as it can show arthritic signs before the appearance of hard tissue changes [Swennen et al., 2006; Pedersen et al., 2008; Müller et al., 2009]. However, CBCT is more adequate in detecting changes in shape (flattening, erosion, osteophyte) than in MRI, which may be because MRI has a larger slice thickness (more than 3 mm compared to 0.4 mm in CBCT) in clinical use, as well as the possible presence of fibrous tissues inside the TMJ and the close proximity of the lateral pterygoid muscle to the articular surface of the condyle which are factors that could decrease the precision in the MRI analysis [Alkhader et al., 2010].
Aim
The aim of this study was to assess the presence of osseous destruction characteristics by CBCT of the TMJ mandibular condyles because of JIA and to compare these characteristics with a group of patients without JIA.
Material and methods
In this cross-sectional observational study, whereby CBCTs of 65 (130 joints) patients with a confirmed JIA diagnosis (referred from the Paediatric Clinical University Hospital’s Rheumatology department) and 30 (60 joints) control group i.e. patients without JIA (obtained from the Orthodontic department of the Stomatology Institute) were evaluated by the author.
The inclusion criteria were children up to the age of 17 and with a confirmed diagnosis of JIA. For the control group the inclusion criteria were also the age up to 17 years and having an indication for a CBCT such as impacted canines. The JIA group had 45 females and 20 males and the control group had 24 females and 6 males. The mean age of the JIA group was 14.2 years (range 9–17), the mean age of the control group was 13.67 years (range 10–17). CBCT was used for the examination and evaluation of the mandibular condyle and verifying whether there was any radiographic evidence of disorders or abnormalities in these condyles.
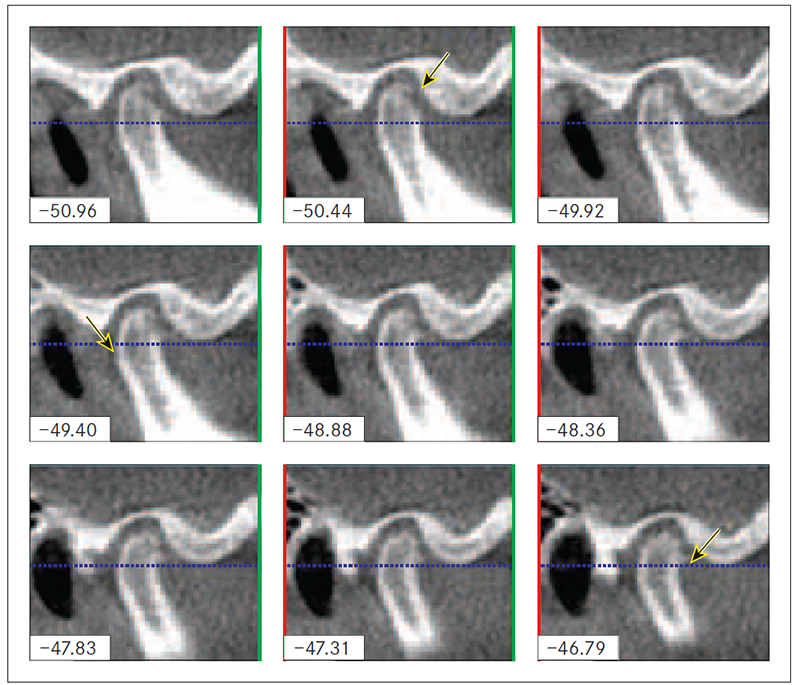
Structural radiologic characteristics of the condyles were assessed in the sagittal, coronal and axial planes. The CBCT images assessed the condyles for presence or absence of the following; hypoplasia, flattening, subcortical sclerosis, subcortical cyst, surface erosion, osteophyte, generalised sclerosis, deviation in form, and bony ankylosis (Figure 1 for a sagittal view of a condyle with erosion, cyst, and osteophyte).
This study was conducted in the Orthodontic Department of Rīga Stradiņš University’s Stomatology Institute, the Paediatric Clinical University Hospital’s Rheumatology Department in referring the JIA patients in order to carry out a full assessment of the TMJ and obtain CBCT scans.
Figure 1. Sagittal view of condyle with erosion, cyst, and osteophyte (highlighted by the arrows)
For the CBCT images, the data was processed and analysed with I-CAT Vision equipment (Imaging Sciences International, Inc. Hatfield PA, USA). The equipment used standardised protocol: voltage: 120 KV, current: 38 mA, field of view: 17 cm, resolution: 0.4 voxels, radiation dose 36 μSv. Statistical data analysis was performed to evaluate the distribution of the radiologic osseous structural changes in the two study groups. Data was entered into MS Excel and processed by SPSS (version 20.0, SPSS Inc., Chicago, Il, USA). Chi-squared and Fisher’s exact tests were used to calculate statistical significances between changes in the condyles of healthy individuals and JIA patients, as well as in frequencies of affected condyles in different groups.
This study was approved by the Ethics Committee of Rīga Stradiņš University (Decision accepted with the principles laid down in the Declaration of Helsinki).
Results
The prevalence of mandibular condyles with evident radiologic destruction characteristics, and a comparison between the JIA and control group for the right and left sides are shown in Tables 1 and 2 (Table 1 for females and Table 2 for males). The flattening of the condyles was seen significantly more often in JIA patients compared to the controls (82.8 %) and more in females than in males. The surface erosion of condyles was seen only in the JIA group and affected 58.7 % and in 63.0 % of the right and left side, respectively, in females. The osteophytes were a less frequently seen destruction characteristic and affected 39.1 % and 30.4 % of the right and left side, respectively, in JIA patients only. Other destruction characteristics were observed less frequently (Table 1 and Table 2).
Table 1. Comparison of frequency of radiologic characteristics of mandibular condyle between JIA group and control group for the right and left sides in females
| Characteristic (condylar head) | Right Side | Left side | ||||
|---|---|---|---|---|---|---|
| JIA | Control | P value | JIA | Control | P value | |
| Hypoplasia | 32.6 | 28.3 | 0.038* | 8.3 | 4.2 | 0.025* |
| Surface flattening | 87.0 | 91.3 | < 0.0001* | 4.2 | 8.3 | < 0.0001* |
| Subcortical sclerosis | 28.3 | 23.9 | 0.003* | 0 | 0 | 0.012* |
| Subcortical cyst | 17.4 | 19.6 | 0.044* | 0 | 0 | 0.023* |
| Surface erosion | 58.7 | 63.0 | < 0.0001* | 0 | 0 | < 0.0001* |
| Osteophyte | 39.1 | 30.4 | < 0.0001* | 0 | 0 | 0.001* |
| Generalised sclerosis | 2.2 | 2.2 | 1.000 | 0 | 0 | 1.000 |
| Deviation in form | 10.9 | 13.0 | ― | 0 | 0 | ― |
| Bony ankylosis | 4.3 | 0 | 0.157 | 0 | 0 | 0.087 |
* With statistical significance (p < 0.05).
Table 2. Comparison of frequency of radiologic characteristics of mandibular condyle between JIA group and control group for the right and left sides in males
| Characteristic (condylar head) | Right Side | Left side | ||||
|---|---|---|---|---|---|---|
| JIA | Control | P value | JIA | Control | P value | |
| Hypoplasia | 21.1 | 0 | 0.540 | 21.1 | 0 | 0.540 |
| Surface flattening | 68.4 | 0 | 0.005* | 89.5 | 0 | < 0.0001* |
| Subcortical sclerosis | 26.3 | 0 | 0.289 | 5.3 | 0 | 1.000 |
| Subcortical cyst | 15.8 | 0 | 0.554 | 15.8 | 0 | 0.554 |
| Surface erosion | 42.1 | 0 | 0.129 | 47.4 | 0 | 0.057 |
| Osteophyte | 5.3 | 0 | 1.000 | 21.1 | 0 | 0.540 |
| Generalised sclerosis | 0 | 0 | ― | 0 | 0 | ― |
| Deviation in form | 0 | 0 | ― | 0 | 0 | ― |
| Bony ankylosis | 0 | 0 | 1.000 | 0 | 0 | ― |
* With statistical significance (p < 0.05).
Discussion
A limitation of this study is that there is a time lapse between the diagnosis and the taking of the CBCT, which could have affected the degree of severity of the radiologic characteristics observed. Unfortunately, due to the design of this study, the examiner (Hadeel Al-Shwaikh) was aware of the diagnosis of the patients, therefore some bias could have occurred. The examiner was not a qualified radiologist; however, she was calibrated with an experienced radiologist before conducting this study. The clinical symptoms of the JIA patients were not taken into account since this was not the aim of the study. To achieve more informative and reliable results, a more selective group of JIA patients, or the severity and time elapsed between the taking of the CBCT and diagnosis have to be considered.
To be able to comprehend the age specificities of the mandibular condyle, it is necessary to evaluate the CBCT images from a group of patients without JIA. A normal condyle is defined as being oval and rounded in shape in the axial plane and being convex, round, or flat in the coronal plane [Yale et al., 1966]. In the sagittal plane, the condyle should be round with the cortical outline intact, smooth, and even in thickness [Brooks et al., 1992; Loubele et al., 2009].
We observed that in our control group, condyle hypoplasia condyle surface flattening were present. The presence of these morphological features seen in CBCT could be due to the fact that condyles and the TMJ in general, undergo continuous functional remodeling as the child is growing and, therefore, condylar surface flattening and some perceived condylar surface erosions might in fact be nothing more than a normal physiological process [Brooks et al., 1992]. Karlo et al. suggested that the condyle in childhood changes form round to oval and until the age of 7, the condyle will have formed to 80 % [Karlo et al., 2010]. Thus, physiological growth may explain the number of patients with these characteristics within the control group.
The involvement of the TMJ in JIA patients is described as containing heterogeneous deformities, which may be a result of local growth disturbances, remodeling, or healed destructive processes [Bache, 1964; Larheim et al., 1981; Arvidsson et al., 2010]. The most prevalent radiologic characteristic observed in our study concerning the structure and morphology of the JIA condyles were surface flattening, surface erosion, and osteophytes, which is corroborated by existing literature [Bache, 1964; Larheim et al., 1981; Arvidsson et al., 2010].
Arvidsson et al. in 2010 described the long-term radiologic findings, which were assessed by a different approach in terms of the methodology; by MRI and conventional computed tomography (CT) in adults with long-standing JIA. Concerning the CT findings, they looked for abnormal shape or size of the TMJ condyle cortical bone defects such as superior condylar concavity, cortical defects with and without a sclerotic margin and anterior condyle position in a closed mouth position. They also found bifid condyles, hyperplasia of condyles and fossa eminences as well as subchondral cysts of the condyle [Arvidsson et al., 2010]. These results are explained by the fact that adult patients were studied and so we cannot accurately compare those findings of hyperplasia and bifid condyles with our JIA sample.
A study conducted by Sidiropoulou-Chatzigianni et al. (2008) evaluated the presence of condylar destruction and lesions in orthopantomograms (OPG) of 66 children with JIA diagnosis. They also determined whether destructions were found uni- or bilaterally. The study showed that 50 % of the children had some form of condylar destruction, and if they were present unilaterally, they seemed to favour the right TMJ condyle, which was to some degree in accordance with the results of this research since condylar hypoplasia, subcortical sclerosis and bony ankylosis were features, which seemed to favour the right condyle. However, the authors did not further classify these “lesions and destructions”; they simply indicated if there was any presence of any form of destruction [Sidiropoulou-Chatzigianni et al., 2008]. Again, the radiologic method differs from our study.
Hu et al. (1995) observed condyle surface erosion on conventional CT images of JIA affected children thus supporting our findings. One year later, Hu et al. published another report using CT and found that bony abnormalities of the TMJ in children with JIA occurred in almost two-thirds of children and they had “variable stages” of condyle degeneration, the type of degeneration was not mentioned [Hu et al., 1996]. Kitai et al. used CT and MRI to observe the TMJ and they reported similar results [Kitai et al., 2002] to Hu et al. Scolozzi et al. performed a study using both CT and MRI to lead to diagnosis of JIA and noticed multiple articular bony changes [Scolozzi et al., 2005], consolidating the findings of this study.
Huntjens et al. (2008) inspected CBCT images of JIA patients and observed several condylar destruction characteristics ranging from minor erosions of condyle to virtually complete deformation of condyle [Huntjens et al., 2008]. In 2010, Farronato et al. used CBCT to quantify the TMJ osseous destruction in JIA affected patients and concluded that with the advent of CBCT a more accurate visualisation of early morphologic changes in the TMJ is attainable [Farronato et al., 2010].
The present study has shown that CBCT is an effective tool for evaluating the type(s) of osseous destruction of the TMJ mandibular condyle because of JIA. As the reviewed literature has proven, it has become increasingly apparent that there is insufficiently published data regarding the type of the mandibular condyle osseous destruction in children because of JIA by using CBCT as well as a comparison of this group of patients to the control group.
Conclusions
CBCT images clearly showed that in the JIA group the most prevalent osseous destruction characteristics of the mandibular condyle were condylar surface flattening, followed by surface erosion and osteophyte. It seems that there is no pattern of the destruction for both sides symmetrically. In some control patients, mild condyle surface flattening and hypoplasia were observed, which could be due to physiological growth and development of TMJ.
References
- Alexiou K., Stamatakis H., Tsiklakis K. Evaluation of the severity of temporomandibular joint osteoarthritic changes related to age using cone beam computed tomography // Dentomaxillofacial Radiology, 2009; 38: 141–147.
- Alkhader M., Ohbayashi N., Tetsumura A., Nakamura S., et al. Diagnostic performance of magnetic resonance imaging for detecting osseous abnormalities of the temporomandibular joint and its correlation with cone beam computed tomography // Dentomaxillofacial Radiology, 2010; 39 (5): 270–276.
- Arvidsson L. Z., Smith H. J., Berit F., Larheim T. A. Temporomandibular joint findings in adults with long-standing juvenile idiopathic arthritis: CT and MR imaging assessment // Radiology, 2010; 256 (1).
- Bache C. Mandibular growth and dental occlusion in juvenile rheumatoid arthritis // Acta Rheumatology Scandinavia, 1964; 10: 142–153.
- Billiau A. D., Hu Y., Verdonck A., Carels C., et al. Temporomandibular joint arthritis in juvenile idiopathic arthritis: prevalence, clinical and radiological signs, and relation to dentofacial morphology // Journal of Rheumatology, 2007; 34 (9): 1925–1933.
- Brooks S. L., Westesson P. L., Eriksson L., Hansson L. G., et al. Prevalence of osseous changes in the temporomandibular joint of asymptomatic persons without internal derangement // Oral Surgery Oral Medicine Oral Pathology, 1992; 73 (1): 118–122.
- Cassidy J. T. Treatment of children with juvenile rheumatoid arthritis // New England Journal of Medicine, 1986; 314 (20): 1312–1314.
- Dahlstrom L., Lindvall A. M. Assessment of temporomandibular joint disease by panoramic radiography: Reliability and validity in relation to tomography // Dentomaxillofacial Radiology, 1996; 25: 197–201.
- Farronato G., Garagiola U., Carletti V., Cressoni P., et al. Change in condylar and mandibular morphology in juvenile idiopathic arthritis: Cone beam volumetric imaging // Minerva Stomatology, 2010; 59: 519–534.
- Ferraz A. M., Devito K. L., Guimarães J. P. Temporomandibular disorder in patients with juvenile idiopathic arthritis: Clinical evaluation and correlation with the findings of cone beam computed tomography // Oral Surgery Oral Medicine Oral Pathology Oral Radiology, 2012; 114 (3): e51–7.
- Fjeld M., Arvidsson L., Smith H. J., Flatø B., et al. Relationship between disease course in the temporomandibular joints and mandibular growth rotation in patients with juvenile idiopathic arthritis followed from childhood to adulthood // Pediatric Rheumatology Online Journal, 2010; 22 (8): 13.
- Garagiola U., Mercatali L., Bellintani C., Fodor A., et al. Change in condylar and mandibular morphology in juvenile idiopathic arthritis: Cone beam volumetric imaging // Fogorv Sz., 2013; 106 (1): 27–31.
- Hu Y. S., Schneiderman E. D. The temporomandibular joint in juvenile rheumatoid arthritis: I. Computed tomographic findings // Pediatric Dentistry, 1995; 17: 46–53.
- Hu Y. S., Schneiderman E. D., Harper R. P. The temporomandibular joint in juvenile rheumatoid arthritis: Part II. Relationship between computed tomographic and clinical findings // Pediatric Dentistry, 1996; 18: 312–319.
- Huntjens E., Kiss G., Wouters C., Carels C. Condylar asymmetry in children with juvenile idiopathic arthritis assessed by cone-beam computed tomography // European Journal of Orthodontics, 2008; 30 (6): 545–551.
- Karlo C. A., Stolzmann P., Habernig S., Müller L. Size, shape and age-related changes of the mandibular condyle during childhood // European Radiology, 2010; 20 (10): 2512–2517.
- Kitai N., Kreiborg S., Murakami S., Bakke M., et al. A three-dimensional method of visualizing the temporomandibular joint based on magnetic resonance imaging in a case of juvenile chronic arthritis // International Journal of Paediatric Dentistry, 2002; 12: 109–115.
- Larheim T. A., Haanaes H. R., Dale K. Radiographic temporomandibular joint abnormality in adults with micrognathia and juvenile rheumatoid arthritis // Acta Radiologica Diagnostics (Stockholm) 1981; 22 (4): 495–504.
- Loubele M., Bogaerts R., Van Dijck E., Pauwels R., et al. Comparison between effective radiation dose of CBCT and MSCT scanners for dentomaxillofacial applications // European Journal of Radiology, 2009; 71 (3): 461–468.
- Müller L., Kellenberger C. J., Cannizzaro E., Ettlin D., et al. Early diagnosis of temporomandibular joint involvement in juvenile idiopathic arthritis: A pilot study comparing clinical examination and ultrasound to magnetic resonance imaging // Rheumatology (Oxford), 2009; 48 (6): 680–685.
- Pedersen T. K., Küseler A., Gelineck J., Herlin T. A prospective study of magnetic resonance and radiographic imaging in relation to symptoms and clinical findings of the temporomandibular joint in children with juvenile idiopathic arthritis // Journal of Rheumatology, 2008; 35 (8): 1668–1675.
- Petersson A. What you can and cannot see in TMJ imaging – an overview related to the RDC/TMD diagnostic system // Journal of Oral Rehabilitation, 2010; 37: 771–778.
- Pirttiniemi P., Kantomaa T., Sorsa T. Effect of decreased loading on the metabolic activity of the mandibular condylar cartilage in the rat // European Journal of Orthodontics, 2004; 26 (1): 1–5.
- Ringold S., Cron R. Q. The temporomandibular joint in juvenile idiopathic arthritis: Frequently used and frequently arthritic // Pediatric Rheumatology Online Journal, 2009; 7: 11.
- Scolozzi P., Bosson G., Jaques B. Severe isolated temporomandibular joint involvement in juvenile idiopathic arthritis // Journal of Oral Maxillofacial Surgery, 2005; 63: 1368–1371.
- Sidiropoulou-Chatzigianni S., Papadopoulos M. A., Kolokithas G. Mandibular condyle lesions in children with juvenile idiopathic arthritis // Cleft Palate Craniofacial Journal, 2008; 45 (1): 57–62.
- Swennen G. R., Schutyser F. Three-dimensional cephalometry: Spiral multi-slice vs cone-beam computed tomography // American Journal of Orthodontics and Dentofacial Orthopedics, 2006; 130 (3): 410–416.
- Te Veldhuis E. C., Te Veldhuis A. H., Koudstaal M. J. Treatment management of children with juvenile idiopathic arthritis with temporomandibular joint involvement: A systematic review // Oral Surgery Oral Medicine Oral Pathology Oral Radiology, 2014; 117 (5): 581–589.e2.
- Twilt M., Movers S. M., Arends L. R., ten Cate R., et al. Temporomandibular involvement in juvenile idiopathic arthritis // Journal of Rheumatology, 2004; 31 (7): 1418–1422.
- Yale S. H., Allison B. D., Hauptfuehrer J. D. An epidemiological assessment of mandibular condyle morphology // Oral Surgery Oral Medicine Oral Pathology, 1966; 21 (2): 169–177.